Issue Category: Public Health Funding
Nuevo informe mide la preparación para emergencias de los estados y hace recomendaciones sobre cómo fortalecer el sistema de salud pública de la nación
Se necesita una inversión sostenida en infraestructura de salud pública y preparación para proteger vidas durante brotes de enfermedades y desastres naturales
(Washington, DC – 23 de marzo de 2023) – A medida que los brotes de enfermedades infecciosas y los fenómenos meteorológicos extremos amenazan la salud de más estadounidenses, un nuevo informe muestra la necesidad de fortalecer la preparación para emergencias de salud pública a nivel nacional y estatal.
Ready or Not 2023: Protecting the Public’s Health from Diseases, Disasters, and Bioterrorism, informe publicado hoy por Trust for America’s Health, mide la preparación de los estados para responder a un espectro de emergencias de salud y brindar servicios de salud pública continuos. El informe brinda a los funcionarios de salud federales y estatales y a los formuladores de políticas datos procesables y recomienda políticas para mejorar la preparación para emergencias de la nación en un momento en que las emergencias de salud están aumentando. Durante el 2022, los Estados Unidos superó el millón de muertes debido al COVID-19 y experimentó tasas decrecientes de vacunas de rutina y una prevalencia creciente de información errónea sobre la salud. Además, el año pasado fue el octavo año consecutivo en que los Estados Unidos experimentó 10 o más desastres relacionados con el clima con un impacto de mil millones de dólares.
El informe clasifica a los estados y al Distrito de Columbia en tres niveles de desempeño para la preparación para emergencias de salud: alto, medio y bajo. El informe de este año colocó a 19 estados y DC en el nivel de alto rendimiento, 16 estados en el nivel de rendimiento medio y 15 estados en el nivel de bajo rendimiento.
Nivel alto: 19 estados y DC
CO, CT, DC, DE, FL, GA, KS, ME, MD, MA, MS, NJ, NC, OH, PA, UT, VT, VA, WA, WI
Nivel medio: 16 estados
Alaska, Alabama, AR, CA, IA, ID, IL, IN, MO, ND, NE, NH, NY, RI, SC, TX
Nivel bajo: 15 estados
AZ, HI, KY, LA, MI, MN, MT, NM, NV, OK, OR, SD, TN, WV, WY
“Una inversión mayor y sostenida en infraestructura de salud pública, preparación para emergencias y equidad en salud salvará vidas”, dijo J. Nadine Gracia, M.D., MSCE, presidenta y directora ejecutiva de Trust for America’s Health. “Los funcionarios federales, estatales y locales, así como los líderes de los sectores empresarial y de atención de la salud deben utilizar nuestros hallazgos para identificar y abordar las brechas en la preparación de la salud pública. No hacerlo significará que el país no estará tan preparado como debe estar para la próxima emergencia de salud pública”.
Las áreas de fuerte desempeño incluyen:
- La mayoría de los estados han hecho preparativos para expandir la capacidad de los laboratorios de atención médica y salud pública en una emergencia.
- La mayoría de los estados están acreditados en las áreas de salud pública o manejo de emergencias. Algunos estados están acreditados en ambos.
- La mayoría de los residentes de EE. UU. que recibieron el agua de su hogar a través de un sistema de agua comunitario tenían acceso a agua segura. Sin embargo, las fallas recientes en el sistema de agua en Jackson, Mississippi y Newark, Nueva Jersey demuestran la importancia de prestar atención continua a la integridad de los sistemas de agua municipales.
Las áreas que necesitan atención incluyen:
- Muy pocas personas se vacunaron contra la gripe estacional el año pasado a pesar de la mejora significativa en las tasas de vacunación contra la gripe en los últimos años. Durante la temporada de influenza 2021-2022, el 51 % de los estadounidenses de 6 meses o más recibieron una vacuna contra la influenza, muy por debajo de la meta del 70 % establecida por Healthy People 2030.
- Solo la mitad de la población de los Estados Unidos cuenta con un sistema integral de salud pública. Los sistemas integrales de salud pública aseguran que los servicios de salud necesarios estén disponibles para todos los residentes.
- Solo el 26 por ciento de los hospitales en los estados, en promedio, obtuvo una calificación de seguridad del paciente de máxima calidad en el 2022. Las puntuaciones de seguridad hospitalaria miden el desempeño en temas tales como las tasas de infecciones asociadas con la atención médica, la capacidad de cuidados intensivos y una cultura general de prevención de errores.
El informe contiene recomendaciones para acciones políticas que crearían un sistema de salud pública más sólido en todos los niveles, que incluyen:
- La Administración, el Congreso y los legisladores estatales deben modernizar la infraestructura de salud pública, incluso mediante la inversión de $4500 millones anuales para respaldar las capacidades básicas de salud pública. Además, el Congreso debe continuar aumentando los fondos para el acuerdo cooperativo de preparación para emergencias de salud pública y la modernización de datos de salud pública para permitir una detección más temprana y precisa de amenazas emergentes para la salud.
- Los formuladores de políticas en todos los niveles deben actuar para proteger y fortalecer a las autoridades de salud pública y deben priorizar la recuperación de la confianza en las agencias y líderes de salud pública.
- El Congreso y las legislaturas estatales deben invertir en comunicaciones efectivas de salud pública, incluida la lucha contra la desinformación.
- El Congreso y los estados deben garantizar la cobertura del primer dólar para todas las vacunas recomendadas bajo seguros comerciales y para personas sin seguro. Los estados deben minimizar las exenciones de vacunas para niños en edad escolar, y los centros de atención médica deben aumentar las tasas de vacunación para los trabajadores de la salud.
- El Congreso y los estados deben otorgar licencias remuneradas con protección laboral a los empleados debido a enfermedades o demandas de cuidado familiar.
- El Congreso y los estados deben invertir en políticas y capacidad para abordar los determinantes sociales de la salud, como vivienda segura, acceso al transporte y acceso a alimentos saludables.
- El Congreso debe financiar toda la empresa de contramedidas médicas (MCM), incluida la distribución y dispensación de MCM. El Congreso también debería crear incentivos para nuevos productos para prevenir y combatir las infecciones resistentes a los antibióticos.
- El Congreso y los estados deben fortalecer la preparación para el cambio climático, el clima extremo y las amenazas a la salud ambiental.
Lea el informe completo en: Ready or Not 2023
Trust for America’s Health es una organización no partidista y sin fines de lucro que promueve la salud óptima para cada persona y comunidad y hace de la prevención de enfermedades y lesiones una prioridad nacional.
Legislative Priorities for the 118th Congress
New Report: Nation’s Chronic Lack of Investment in Public Health Puts Americans’ Lives and Livelihoods at Risk
COVID-19 emergency funding was critical to initial pandemic response but did not address nation’s long-standing underinvestment in public health; $4.5 billion in annual infrastructure funding is needed
(Washington, DC – July 28, 2022) – Chronic underfunding has created a public health system that cannot address the nation’s health security needs, its persistent health inequities, as well as emerging threats, and, was a contributing factor in the inadequate response to the COVID-19 pandemic, according to a report, The Impact of Chronic Underfunding on America’s Public Health System: Trends, Risks, and Recommendations, 2022, released today by Trust for America’s Health.
Lack of funding in core public health programs slowed the response to the COVID-19 pandemic and exacerbated its impact, particularly in low-income communities, communities of color, and for older Americans – populations that experience higher rates of chronic disease and have fewer resources to recover from an emergency. TFAH is one of numerous organizations within the public health community calling for an annual $4.5 billion investment in public health infrastructure at the state, local, tribal, and territorial levels.
This annual report examines federal, state, and local public health funding trends and recommends investments and policy actions to build a stronger public health system, prioritize prevention, and address the ways in which social and economic inequities create barriers to good health in many communities.
“As we navigate the next stages of the pandemic and beyond, it is critical that we modernize public health data infrastructure, grow and diversify the public health workforce, invest in health promotion and prevention programs, and reduce health inequities. Investments in public health are needed in every community but should particularly be directed to those communities, which due to the impacts of structural racism, poverty, systemic discrimination, and disinvestment are placed at greatest risk during a health emergency,” said Dr. Gracia.
Emergency funding is not sufficient to address system weaknesses created by chronic underfunding
State and local public health agencies managed two divergent realities during 2021. Short-term funding was up significantly as the federal government provided funding to states and localities in an effort to control the pandemic. But this funding was one-time money and often specifically tied to COVID-19. Most of it could not be used to address longstanding deficits in the public health system, including ensuring the provision of basic public health services, replacing antiquated data systems, and growing the public health workforce. An October 2021 analysis conducted by the de Beaumont Foundation and the Public Health National Center for Innovations, found that state and local health departments need an 80 percent increase in the size of their workforce to be able to provide comprehensive public health services to their communities.
Another challenge for state and local health departments is that emergency response funding, while critical during the emergency, is too late to build prevention and preparedness programs, programs that must be in place before an emergency if they are going to protect lives. To be adequately prepared for the next public health emergency, the nation needs to sustain higher levels of public health funding and provide more flexible funding.
“Emergency funding is important but not sufficient to fill the longstanding gaps in public health investments. The ‘boom-and-bust’ cycle of public health funding has meant that the system does not have the tools or workforce to modernize and respond to the range of threats impacting our communities,” said J. Nadine Gracia, M.D., MSCE, President and CEO of Trust for America’s Health.
Funding for two key emergency preparedness and response programs are down sharply over the past two decades:
- The U.S. Centers for Disease Control and Prevention (CDC) is the country’s leading public health agency and the primary source of funding for state, local, tribal, and territorial health departments. CDC’s annual funding for Public Health Emergency Preparedness (PHEP) programs increased slightly between FY 2021 and FY 2022, from $840 million to $862 million, but has been reduced by just over one-fifth since FY 2002, or approximately in half when adjusted for inflation.
- The Hospital Preparedness Program, administered by the U.S. Department of Health and Human Services’ Office of the Assistant Secretary for Preparedness and Response, is the primary source of federal funding to help healthcare systems prepare for emergencies. It has experienced a nearly two-thirds reduction over the last two decades when adjusted for inflation.
Funding for health promotion, prevention, and equity also need sustained growth
As a nation, we spent $4.1 trillion on health in 2020 but only 5.4 percent of that spending targeted public health and prevention. Notably, this share nearly doubled last year as compared to 2019 – due to short-term COVID-19 response funding – but is still grossly inadequate and likely to return to pre-pandemic levels if the historic pattern of surging funding for public health during an emergency but neglecting it at other times resumes. Inadequate funding means that effective public health programs, such as those to prevent suicide, obesity, and environmental health threats, only reach a fraction of states. This longstanding neglect contributes to high rates of chronic disease and persistent health inequities.
Recommendations for policy actions
The report calls for policy action by the administration, Congress, and state and local officials within four areas:
Substantially increase core funding to strengthen public health infrastructure and grow the public health workforce, including increasing CDC’s base appropriation and modernizing the nation’s public health data and disease tracking systems.
Invest in the nation’s health security by increasing funding for public health emergency preparedness, including within the healthcare system, improving immunization infrastructure, and addressing the impacts of climate change.
Address health inequities and their impact on root causes of disease by addressing the social determinants of health that have an outsized impact on health outcomes.
Safeguard and improve health across the lifespan. Many programs that promote health and prevent the leading causes of disease, disability, and death have been long neglected and do not reach all states or the populations most at risk. Reinvigorating programs that stem chronic disease, support children and families, and prevent substance misuse and suicide should be a top priority.
Read the full report
Nuevo Reporte: La Falta Reiterada de inversión en Salud Pública Por Parte de la Nación, Pone en Riesgo La Vida y Los Medios De Subsistencia De Los Estadounidenses
Los Fondos de Emergencia del COVID-19 fue una respuesta fundamental desde un principio, pero no lo suficiente efectiva para atender el problema que viene acarreando el país debido a la falta de inversión en la salud pública; Se necesitan $ 4.5 mil millones en fondos anuales
(Washington, DC – 28 de julio del 2022) – La insuficiencia crónica de fondos ha creado un sistema de salud pública que no logra cubrir las necesidades de seguridad de salud de la nación, las persistentes desigualdades en la salud, así como las amenazas emergentes, y fue uno de los factores que contribuyó a la respuesta inadecuada a la pandemia de COVID-19, según un informe, The Impact of Chronic Underfunding on America’s Public Health System: Trends, Risks, and Recommendations, 2022, publicado hoy por Trust for America’s Health.
“El financiamiento de emergencia es importante pero no suficiente para llenar los vacíos de larga data en las inversiones en salud pública. El ciclo de ‘auge y caída’ de la financiación de la salud pública demuestra que el sistema no tiene las herramientas o la fuerza laboral para modernizarse y responder a las diversas amenazas que afectan a nuestras comunidades”, dijo J. Nadine Gracia, M.D., MSCE, presidente y directora ejecutiva de Trust for America’s Health.
Este informe anual examina las tendencias de financiación de la salud pública a nivel federal, estatal y local, recomendando inversiones y acciones políticas para construir un sistema de salud pública más fuerte, dándole prioridad a la prevención, abordando temas como las desigualdades sociales y económicas las cuales crean barreras para lograr un buen sistema de salud en muchas comunidades.
La falta de fondos para programas básicos de salud pública desaceleró la respuesta a la pandemia de COVID-19 y exacerbó su impacto, particularmente en las comunidades de bajos ingresos, comunidades de color y en los estadounidenses de avanzada edad los cuales son las poblaciones que representan las tasas más altas de enfermedades crónicas y tienen menos recursos para recuperarse de una emergencia. TFAH es una de las numerosas organizaciones dentro de la comunidad de salud pública que solicita una inversión anual de $4500 millones en infraestructura de salud pública a nivel estatal, local, tribus y territorial.
“A medida que atravesamos nuevas etapas de la pandemia vemos más allá, y se observa que la necesidad fundamental es que se modernice la infraestructura de datos de salud pública, que aumentemos y diversifiquemos la fuerza laboral de salud pública, que se invierta en programas de prevención y promoción de la salud, reduciendo las desigualdades en el sector de la salud. Las inversiones en salud pública son necesarias en todas las comunidades, pero deben dirigirse particularmente a aquellas comunidades que, debido a los impactos del racismo estructural, la pobreza, la discriminación sistémica y la desinversión, se encuentran en mayor riesgo durante una emergencia de salud”, dijo el Dr. Gracia.
El fondo de emergencia no es suficiente para atender las debilidades del sistema creadas por la falta de financiación crónica
Las agencias de salud pública estatales y locales manejaron dos realidades divergentes durante el 2021. La financiación a corto plazo aumentó significativamente ya que el gobierno federal proporcionó fondos de emergencia en respuesta a los estados y localidades en esfuerzo para controlar la pandemia. Pero esta financiación de dinero se realizó sola vez, y en algunos casos específicamente vinculado al COVID-19. Gran parte de este fondo de emergencia no pudo ser utilizada para abordar los déficits de larga data en el sistema de salud pública, los cuales incluían asegurar provisiones para cubrir los gastos básicos de salud pública, sustituir los sistemas desactualizados de datos y aumentar la fuerza laboral de salud pública. Un análisis de octubre del 2021 realizado por la Fundación de Beaumont y el Centro Nacional de Innovaciones de Salud Pública encontró que los departamentos estatales y locales de salud necesitan un aumento del 80 por ciento en el campo de su fuerza laboral para poder brindar servicios integrales de salud pública a sus comunidades.
Otro desafío para los departamentos de salud a nivel estatal y local es que los fondos de emergencias, si bien es una gran ayuda durante la emergencia, es demasiado tarde para trabajar en un plan de preparación y prevención, ya que estos programas deben implementarse antes de una emergencia para proteger vidas. Para estar adecuadamente preparado para la próxima emergencia de salud pública, la nación debe mantener los niveles de fondos más altos respecto a la salud pública y proveer una financiación flexible.
Los fondos de dos programas clave de preparación y respuesta de emergencias se han visto drásticamente reducidos en las últimas dos décadas:
- Los Centros para el Control y la Prevención de Enfermedades (CDC) de EE. UU. son la principal agencia de salud pública del país y la principal fuente de financiación para los departamentos de salud estatales, locales, tribales y territoriales. La financiación anual de los CDC para los programas de preparación para emergencias de salud pública (PHEP, por sus siglas en inglés) aumentó ligeramente entre el año fiscal 2021 y el año fiscal 2022, de $840 millones a $862 millones, pero ha reducido un poco más de una quinta parte desde el año fiscal 2002, ó aproximadamente a la mitad cuando se ajusta por inflación.
- El Programa de Preparación Hospitalaria, administrado por la Oficina del Subsecretario de Preparación y Respuesta del Departamento de Salud y Servicios Humanos de EE. UU., es la fuente principal de financiamiento federal para ayudar a los sistemas de atención médica a prepararse para emergencias. El programa ha sufrido una reducción de casi dos tercios en las últimas dos décadas cuando se ajusta a la inflación.
Los fondos para la promoción de la salud, la prevención y la equidad también necesita un crecimiento sostenido
Como nación, gastamos $4,1 billones en salud en 2020, pero solo el 5,4 % de ese gasto se destinó a la salud pública y la prevención. Notablemente, casi se duplicó la cifra del año pasado en comparación con el 2019. Esto se debe a la respuesta de fondos implementados a corto plazo en respuesta al COVID-19. Sin embargo, esta cifra sigue siendo insuficiente y muy probable que regrese a los niveles en los que se encontraba antes de la pandemia, si el patrón histórico de aumento de fondos para la salud pública aumenta durante otra emergencia, volveremos a estar en la misma situación. La financiación inadecuada significa que los programas efectivos de salud pública, como aquellos para prevenir el suicidio, la obesidad y las amenazas ambientales para la salud, solo llegan a una fracción de los estados. Esta negligencia de larga data contribuye a las altas tasas de enfermedades crónicas y a las persistentes desigualdades en el ámbito de la salud.
“Debemos romper el patrón de invertir solo en el sistema de salud pública durante una emergencia, ya que no permite trabajar en la preparación y prevención. Es muy importante invertir en salud pública y equidad sanitaria de manera continua, incluso en tiempos que no sean de emergencia, para lograr salvar vidas, reduciendo los costos económicos para nuestra nación durante y entre emergencias”, dijo la Dra. Gracia.
Los impactos del racismo estructural, la pobreza, la discriminación y la desinversión son temas que deben de igual manera abordarse mediante inversiones a través de programas que aseguren que cada comunidad tenga acceso a alimentos saludables, vivienda segura, atención médica, transporte, educación y empleo, ya que todos estos factores afectan la salud de las personas.
Recomendaciones para tomar medidas de acción:
El informe exige la adopción de medidas de acción por parte de la administración, el Congreso y funcionarios tanto estatales como locales en cuatro áreas:
Aumentar sustancialmente los fondos básicos para fortalecer la infraestructura de salud pública y desarrollar su fuerza laboral, incluyendo el aumento de la asignación básica de los CDC y la modernización de los sistemas de seguimiento de enfermedades y datos de salud pública de la nación.
Invertir en la seguridad de la salud de la nación, aumentando los fondos de salud pública para la preparación de emergencias de sanidad, mejorando la infraestructura de inmunización y tomando en cuenta los impactos del cambio climático.
Abordar las desigualdades de la salud y su impacto como causas principal de enfermedades abordando los factores sociales de la salud que tienen un impacto descomunal en temas de salud pública.
Proteger y mejorar la salud a través del tiempo en vida. Muchos programas que promuevan la salud y prevengan las principales causas de enfermedad, discapacidad y muerte se han descuidado durante mucho tiempo, además de no estar disponibles en todos los estados ni a las poblaciones que se encuentran en mayor riesgo. Es de vital importancia, activar los programas que frenan las enfermedades crónicas, apoyar a niños y familias para prevenir el uso indebido de sustancias y colocar como máxima prioridad el suicidio.
Lea el reporte completo en: The Impact of Chronic Underfunding on America’s Public Health System: Trends, Risks, and Recommendations, 2022
Trust for America’s Health es una organización no partidista sin fines de lucro que promueve la salud óptima para cada persona y comunidad a través de la acción política y trabaja para hacer de la prevención de enfermedades y lesiones una prioridad nacional.
The Impact of Chronic Underfunding on America’s Public Health System: Trends, Risks, and Recommendations, 2022
Public Health Leaders Discuss the Importance of Sustained Public Health Funding in the Post COVID-19 Landscape
Trust for America’s Health (TFAH) President & CEO J. Nadine Gracia, and Coalition for Health Funding’s (CHF) Executive Director Erin Will Morton issued the following statement regarding the June 22nd Beyond Emergency Funding: Sustaining Public Health Funding in the Post-COVID Landscape discussion.
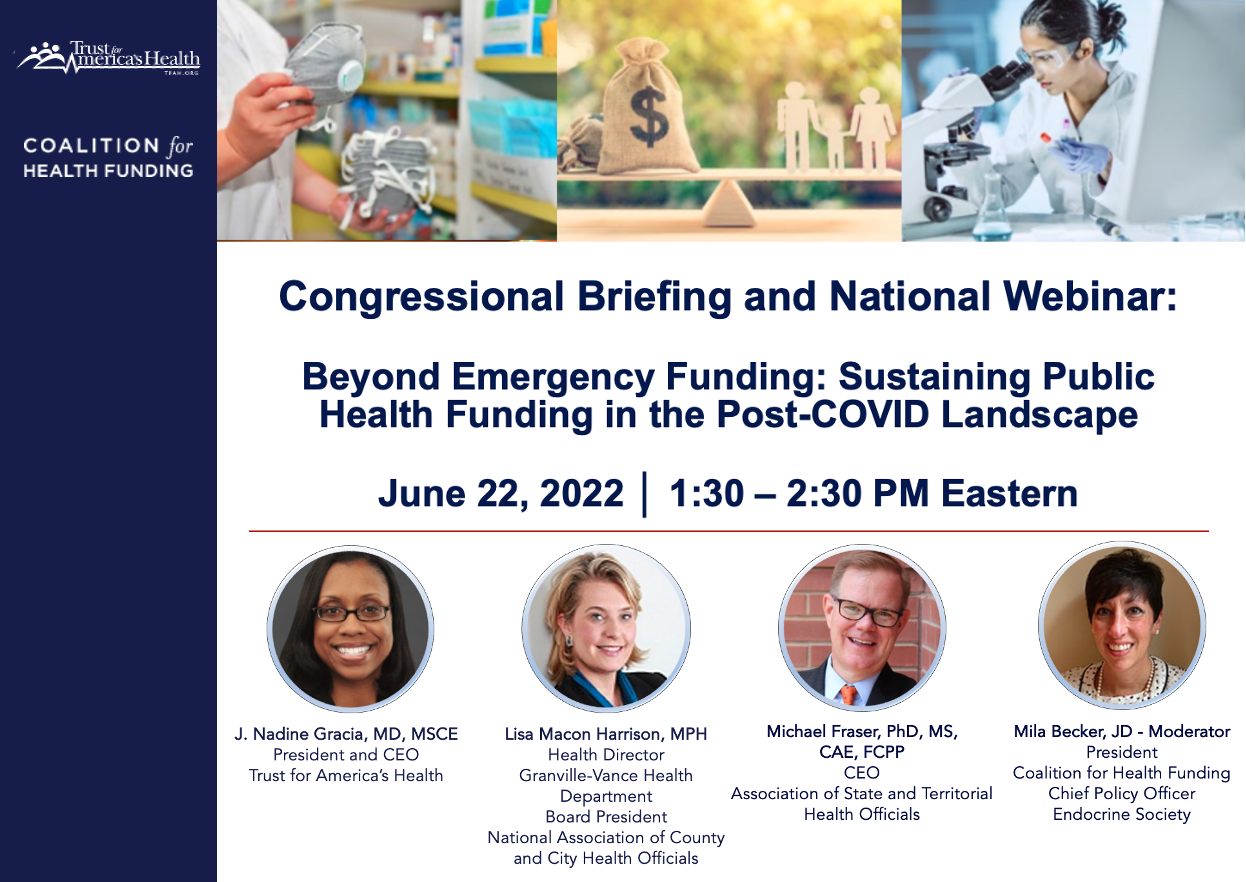
(Washington, DC) — Trust for America’s Health and the Coalition for Health Funding are proud to have hosted the Beyond Emergency Funding: Sustaining Public Health Funding in the Post-COVID Landscape discussion on June 22, 2022. This discussion included three expert panelists; Dr. Gracia, Trust for America’s Health, Lisa Macon Harrison, MPH, Health Director, Granville Vance Public Health (North Carolina), and the current President of the National Association of County and City Health Officials, and Dr. Michael Fraser, Chief Executive Officer, the Association of State and Territorial Health Officials. CHF’s president, Mila Becker, moderated the event.
According to the panelists, the COVID-19 pandemic demonstrated a clear need for a well-funded, broad-based public health infrastructure and workforce at all levels. Our organizations urge lawmakers to increase annual funding to achieve these goals and create a sustainable, long-term funding strategy for public health beyond emergency supplemental funding.
The panelists emphasized the following issues during the session:
- The public health system our country needs cannot be built on the boom-and-bust cycle of emergency funding.
- The system needs long-term, flexible funding. Short term and inflexible funding lines for public health make investing in essential infrastructure, workforce, and cross-cutting approaches to prevention, including addressing the social determinants of health, impossible.
- Public health emergency response is more expensive than funding core public health infrastructure. Billions of dollars spent in the years before the COVID-19 pandemic could have saved the trillions of dollars spent in response to the crisis and would have saved lives.
- We must invest in the public health programs and workforce needed to prevent illness and injury. Doing so would decrease the amount of money now spent on treating preventable disease.
- We must be nimbler and better prepared in order to save lives during the next public health emergency. Core public health services most in need of sustained investment are:
- Modernized data systems that provide real-time data for decision-making.
- Sustained funding for recruitment and retention of a larger and more diverse public health workforce.
- Programs to achieve health equity – during the pandemic many health departments increased their engagement with community leaders and organizations. Those partnerships and networks should be sustained and grown.
- We are approaching a COVID “funding cliff” – emergency funding has been spent or is expiring, but core public health services still need to be provided, particularly in those communities where health inequities were exacerbated by the pandemic.
Listen to the full session at: https://www.tfah.org/webinars-briefings/beyond-emergency-funding/
###
About TFAH
Trust for America’s Health is a non-partisan public health policy, research and advocacy organization that envisions a nation that values the health and well-being of all and where prevention and health equity are foundational to policymaking at all levels of society.
About CHF
The Coalition for Health Funding works to preserve public health investments in the interest of all Americans. Our 81 member organizations together represent more than 100 million patients and consumers, health providers, professionals, and researchers. Coalition for Health Funding (publichealthfunding.org)
Beyond Emergency Funding: Sustaining Public Health Funding in the Post-COVID Landscape
With Congress having spent billions of dollars fighting COVID-19 since early 2020, why should we increase annual funding for public health when we have so many other competing priorities?
TFAH and the Coalition for Health Funding convened experts in public health policy and funding to clearly explain the need for robust, sustainable public health funding and how it must be considered separately from the COVID-19 emergency.