Issue Category: Substance Misuse and Mental Health
Public Health Leaders’ Joint Statement in Response to the Attack on CDC
(Washington, DC – August 14, 2025) – In response to the horrific shooting that occurred on Friday, August 8, targeting the Centers for Disease Control and Prevention (CDC), the public health community stands in solidarity with our CDC colleagues. We denounce acts of harassment, terror, and violence against the public health workforce.
Our hearts break for the family of police officer David Rose who lost his life protecting his community.
Two hundred bullets struck and caused damage to six federal buildings and over 500 rounds were fired at the CDC campus. We are saddened, alarmed, and deeply concerned about the health and safety of our colleagues. The shooting was an attack on an American workplace and on the people and infrastructure that keep us all healthy and safe.
We are committed to working together to support our nation’s dedicated public servants who comprise the public health workforce and call on others to do the same. It is critical to the health of all communities that CDC and all people working in public health across the country are able to continue to make their invaluable contributions to advancing health and well-being without the fear of harassment or violence.
People choosing public health as a profession are committed to advancing our nation’s health and recognize that good health in every community benefits everyone. It is our hope that all Americans will stand with us to support the vital role that CDC and the entire public health workforce play in supporting safety and well-being in every community. Their expertise and commitment to advancing health deserves all Americans’ unwavering support.
American College of Epidemiology
American College of Epidemiology Research and Education Foundation
American Public Health Association
Association of Maternal and Child Health Programs
Association of Public Health Nurses
Association of State and Territorial Dental Directors
Association of State and Territorial Health Officials
Association of State and Territorial Public Health Social Workers
Association of Public Health Laboratories
Association of Schools and Programs of Public Health
Big Cities Health Coalition
CDC Foundation
Council of State and Territorial Epidemiologists
de Beaumont Foundation
National Association of Chronic Disease Directors
National Association of County and City Health Officials
National Association of State Emergency Medical Services Officials
National Network of Public Health Institutes
Prevention Institute
Public Health Accreditation Board
Safe States Alliance
The Kresge Foundation
Trust for America’s Health



![]()






![]()








Marking Three Years of 988 Suicide and Crisis Lifeline Support for People in Need
Since its launch in July 2022, the 988 Suicide and Crisis Lifeline has responded to millions of individuals and has provided immediate support to callers who are in crisis. Still, recent and proposed cuts to the Substance Abuse and Mental Health Services Administration (SAMHSA) and 988 services and the lack of state funding could leave individuals in need or others with fewer options for life-saving help.
The national 988 Suicide and Crisis Lifeline has answered more than 14 million calls, texts, and chats since it was introduced. Call volume to the Lifeline in the first two years of its existence was up 95 percent nationally as compared to calls to the 1-800 system it replaced. In addition, call answer rates have improved and wait times have been reduced.
Still, recent major cuts to agency workforce and a recent decision to end specialized services through 988 for LGBTQIA+ youth and young adults is poised to set that progress back and could have dire consequences.
Brief History
The 988 Suicide and Crisis Lifeline was established by Congress in 2020 and launched officially in 2022 in an effort to enhance the nation’s crisis care system. Established by Congress, 988 was designed to make the previous seven-digit 1-800 suicide prevention lifeline more accessible by creating an easy to remember call number and adding a text option. In 2024, calls and texts began being routed to local crisis centers based on geographic location instead of area codes to help connect users with faster and local support.
In addition, the 988 Lifeline has included specialized support for military veterans, LGTBQIA+ youth, and Spanish-language speakers. To address the disproportionate rates of suicide among American Indian and Alaska Native populations and provide culturally and trauma informed crisis services, the state of Washington offers specialized care for Washington’s American Indian and Alaska Native communities.
People seeking assistance through the 988 Lifeline are able to call, text, and chat through the website with trained professionals at 988 call centers. Counselors either counsel callers through their crisis or direct individuals to acute care in their community.
Research from the American Association of Suicidology found that two-thirds of the people who had suicidal thoughts and reached out via the Lifeline’s online chat reported that the correspondence had been helpful, and 45% reported being less suicidal.
The Need and Demand for the Crisis Lifeline
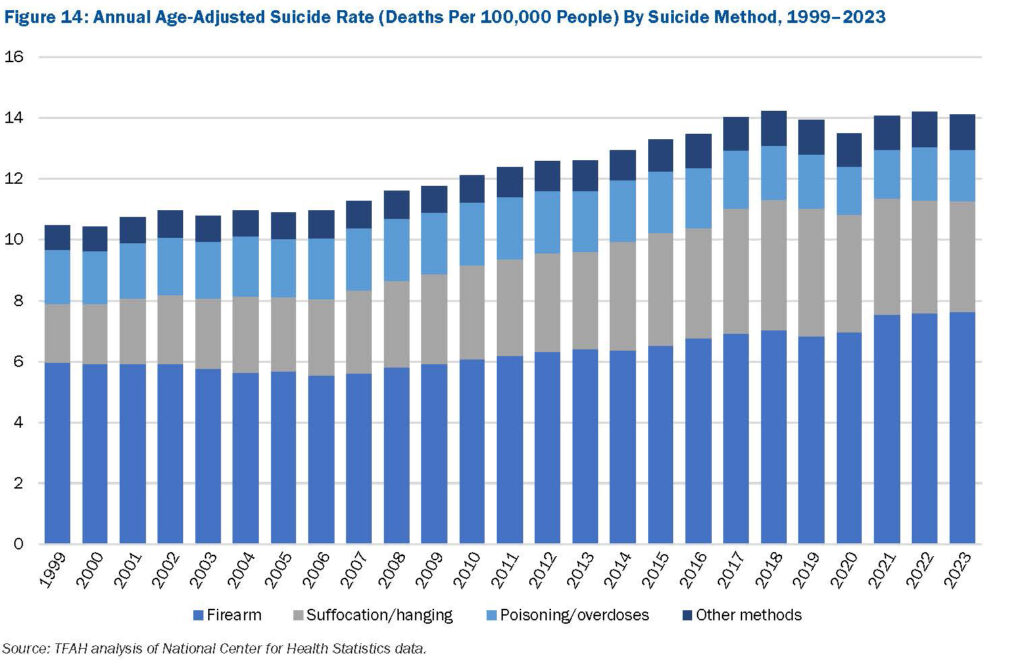
 According to the latest edition of Trust for America’s Health’s Pain in the Nation: The Epidemics of Alcohol, Drug, and Suicide Deaths report, nearly 50,000 Americans of all ages died by suicide in 2023. Although there has been some fluctuation over the past few years, suicide rates have generally been on the rise since 1999. Nearly a half million people died from died by suicide in the U.S. from 2014 to 2023.
According to the latest edition of Trust for America’s Health’s Pain in the Nation: The Epidemics of Alcohol, Drug, and Suicide Deaths report, nearly 50,000 Americans of all ages died by suicide in 2023. Although there has been some fluctuation over the past few years, suicide rates have generally been on the rise since 1999. Nearly a half million people died from died by suicide in the U.S. from 2014 to 2023.
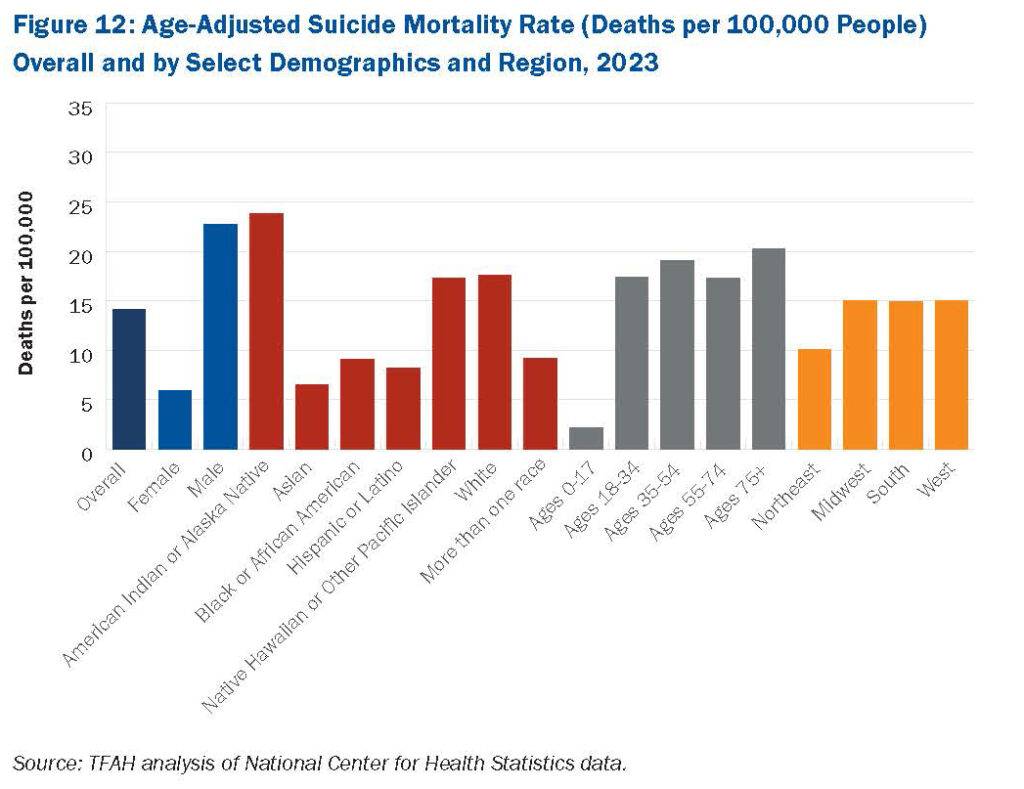
 Some of the highest age-adjusted suicide rates are seen in males and adults ages 75 and older. Suicide rates in rural areas are consistently and significantly higher than urban areas, research shows as well.
Some of the highest age-adjusted suicide rates are seen in males and adults ages 75 and older. Suicide rates in rural areas are consistently and significantly higher than urban areas, research shows as well.
To turn the tide, TFAH urges federal and state policymakers to transform the nation’s mental health and substance use prevention system, in part by strengthening the continuum of crisis intervention supports and programs. TFAH also urges federal agencies to do more to encourage and make people feel more comfortable seeking help with mental health issues, for example by promoting culturally appropriate messaging on mental health screening and treatment to reduce stigma. The 988 Lifeline provides a pathway for states and local communities to implement those recommendations.
Federal and State Support Needs to be Sustained and Increased
The 988 Lifeline is funded primarily through federal funding and is administered by the Substance Abuse and Mental Health Services Administration (SAMHSA). Some states provide additional funding support through their annual budgets and/or telecommunications fees. To date, 16 states are providing funding for their 988 networks. Unfortunately, there are ongoing threats to funding for 988 and suicide prevention services. In March 2025, the Department of Health and Human Services (HHS) announced they would be clawing back $1 billion in SAMHSA funds, including mental health grants many states were applying to 988 suicide lifelines and crisis services. Litigation is putting this clawback on hold in some states. In addition, reductions in force at SAMHSA and the President’s FY 26 Budget Request which proposes to eliminate SAMHSA and significantly reduce mental health programs and funding, could undo progress communities are making in addressing suicide, mental health, and substance use crises.
Where Do We Go From Here?
To continue to support the nation’s crisis services, the following action steps are needed:
- Congress and the Administration should strengthen the 988 Suicide and Crisis Lifeline by maintaining SAMHSA funding for the Lifeline and by restoring the workforce devoted to these services. SAMHSA should also retain the 988 Lifeline’s specialized services, including specialized support for LGBTQIA+ youth and Spanish-language services.
- Congress should also pass the 9-8-8 Implementation Act, which would authorize funding for crisis call centers to purchase or upgrade call center technology, hire and train call center staff, and improve call center operations.
- More states should dedicate funding for the 988 Lifeline and more investments should be made to improve geo-location technology so people that need help are directed to services in their community.
Pain in the Nation 2025: The Epidemics of Alcohol, Drug, and Suicide Deaths
Watch Trust for America’s Health’s (TFAH) for a national webinar and congressional briefing on our recently released report, Pain in the Nation 2025: The Epidemics of Alcohol, Drug, and Suicide Deaths.
TFAH’s Pain in the Nation 2025 report found that over 200,000 Americans died from alcohol, drugs, and suicide in 2023. While this marks a decline from 2022, deaths remain more than double what they were two decades ago. The report highlights improvements in alcohol and drug-related mortality, but disparities persist. Only white Americans saw a drop in overdose deaths, and rates of such deaths remained highest in communities of color. Furthermore, while the reported data represents real progress, current and potential federal funding cuts, public health workforce reductions, and proposed federal agency reorganizations could undermine it.
The briefing included time for Q&A from the audience.
Deaths Due to Drug Overdose and Alcohol Are Down Nationally, But Progress is Uneven Across Population Groups and at Risk Due to Cuts in Federal Health Programs
How can progress be sustained and extended to all communities?
(Washington, D.C. – May 28, 2025) – Deaths due to drug overdose and alcohol misuse were down in the United States in 2023 according to Centers for Disease Control and Prevention (CDC) data and newly released CDC 2024 provisional data predict an unprecedented 27 percent one year drop in overdose deaths. These reductions are encouraging and were likely related to a number of factors including investments in primary prevention, mental health, harm reduction, and overdose prevention programs. However, current and proposed federal budget cuts, public health workforce reductions, and proposed federal agency reorganizations are likely to undermine this progress, according to a new report.
Pain in the Nation 2025: The Epidemics of Alcohol, Drug, and Suicide Deaths, released today by Trust for America’s Health, reports that the combined number of deaths from alcohol, drugs, and suicide in the United States declined in 2023 for the second straight year—after two decades in which such deaths increased at an alarming pace. Still over 200,000 Americans died due to alcohol, drug overdose, or suicide in 2023, twice the rate of such deaths 20 years ago.
The new data highlight the value of investment in mental health and substance use prevention programs – such as ensuring adequate mental health, substance use disorder, and crisis intervention services, access to overdose reversal drugs, and investing in children’s mental health and resilience. The data however also show that much more needs to be done to ensure that the progress against alcohol, drug overdose, and suicide deaths is sustained and that reductions in such deaths are occurring in every community and among all population groups.
“Data show that decades of investment and capacity building in substance use prevention, harm reduction programs, and mental health services have helped reduce associated deaths. The challenge now is to build on these investments and sustain this progress. These programs save lives; their funding should not be cut,” said J. Nadine Gracia, M.D., MSCE, President and CEO of Trust for America’s Health.
Drug overdose rates are declining but still at tragic levels.
In 2023, 105,007 Americans across died from drug overdoses. After precipitous increases in the rate of drug overdose deaths in 2020 and 2021, the 2022 overall overdose mortality rate was virtually unchanged and the 2023 mortality rate was 4 percent lower. Provisional mortality data for 2024 show an unprecedented one-year 27 percent decrease in overdose deaths nationally. Seven states (Louisiana, Michigan, New Hampshire, Ohio, Virginia, West Virginia, and Wisconsin) and Washington D.C. saw the greatest reductions, with declines of 35 percent or more in overdose deaths for the year.
According to public health experts, improved data systems which allow for real-time tracking of substance use and its impacts, the expansion and effectiveness of overdose prevention strategies such as programs to ensure access to naloxone, buprenorphine, and drug-checking tools all played a significant role in bringing down mortality rates.
The improvement was, however, not consistent across all population groups or regions of the country. In 2023, white people were the only racial/ethnic population group that experienced a statistically significant decrease in drug overdose deaths; other population groups had nonsignificant changes or increases. Drug overdose death rates in 2023 were highest among American Indian/Alaska Native people (AI/AN) (65.0 deaths per 100,000 people), adults ages 35 to 54 (57.3 deaths per 100,000 people), Black people (48.5 deaths per 100,000 people), and males (45.6 deaths per 100,000 people).
Alcohol-induced deaths are down.
In 2023, 47,938 Americans died from alcohol-induced causes. The overall age-adjusted alcohol-induced mortality rate decreased by 7 percent from 2022 to 2023 (from 13.5 to 12.6 deaths per 100,000 people). This decrease built on a 6 percent reduction the year prior and crossed nearly all demographic and geographic groups, but such deaths still disproportionately impact some groups. Alcohol-induced death rates in 2023 were highest among AI/AN people (61.5 deaths per 100,000 people), adults ages 55 to 74 (32.5 deaths per 100,000 people), adults ages 35 to 54 (20.2 deaths per 100,000 people), and males (18.1 deaths per 100,000 people).
Suicide deaths unchanged.
The U.S. overall suicide mortality rate remained virtually identical from 2022 to 2023 (14.2 and 14.1 deaths per 100,000 people, respectively). In 2023, 49,316 Americans died from suicide. Age-adjusted suicide rates in 2023 were highest among AI/AN people (23.8 deaths per 100,000 people), males (22.7 deaths per 100,000 people), and adults ages 75 and older (20.3 deaths per 100,000 people).
Budget rescissions and future cuts to prevention programs will cost lives.
While these data demonstrate real progress, the public health community is united in its concern about progress reversals due to cutbacks in federal investment in health promotion, crisis intervention, and overdose prevention programs. For example, staff and funding for the CDC Injury Center have been drastically reduced, and the Center is proposed for elimination in the Administration’s budget request for fiscal year (FY) 2026. The Injury Center conducts research and collects data. Approximately 80 percent of its funding goes to states and other entities for prevention of overdoses, suicide, and adverse childhood experiences (ACEs). Additionally, the Substance Abuse and Mental Health Services Administration (SAMHSA) has experienced major staffing reductions including staff working on the 988 Suicide & Crisis Lifeline, and a potential $1.07 billion funding cut for FY 2026. The Administration has proposed folding some remaining SAMHSA and Injury Center programs into a new Administration for a Healthy America. These actions followed the Administration’s claw-back of billions of dollars in public health funding already at work in states and communities across the country, including for suicide prevention.
The Pain in the Nation report calls for sustained investment in prevention and harm reduction programs and includes recommendations on actions federal and state policymakers should take including:
- Protect and bolster investment in public health and behavioral health systems and injury and violence prevention programs to improve mental health and well-being for all Americans.
- Continue to improve programs, like CDC’s Overdose Data to Action, to track emerging trends by geographic, demographic, and drug type metrics to guide local, state, and national responses and to prevent overdoses and deaths in real time.
- Focus on underlying drivers of substance use disorder through early intervention and prevention policies including expanding resiliency and substance use prevention programs in schools and increasing access to social and mental health services for children and families.
- Maximize harm reduction strategies and substance use disorder treatments to reduce overdose risk, and support efforts to limit access to lethal means of suicide.
- Bolster the continuum of crisis intervention programs and expand the mental health and substance use treatment workforce. Build community capacity to ensure access to mental health and substance use treatment for anyone needing such services.
Read the full report
Trust for America’s Health is a nonprofit, nonpartisan public health policy, research, and advocacy organization that promotes optimal health for every person and community and makes the prevention of illness and injury a national priority. Trust for America’s Health (tfah.org)
Las muertes a causa de sobredosis por drogas y alcohol disminuyen a nivel país, pero el avance es desigual entre los grupos poblacionales y está en riesgo por los recortes en los programas sanitarios a nivel federal
¿Cómo se puede mantener y ampliar el avance para todas las comunidades?
(Washington, D.C., 28 de mayo de 2025). Las muertes a causa de sobredosis por drogas y abuso de alcohol disminuyeron en los Estados Unidos en 2023, según datos de los Centros para el control y prevención de enfermedades (CDC) y de los últimos datos provisorios publicados por los CDC en 2024, en donde que estima una baja sin precedentes del 27 % en un año en las muertes por sobredosis. Estas disminuciones son alentadoras y probablemente se relacionaron con una serie de factores, entre los que se incluyen las inversiones en prevención primaria, la salud mental, la reducción de riesgos y los programas de prevención de sobredosis. No obstante, los recortes presupuestarios actuales y propuestos a nivel federal, la reducción de la fuerza laboral de la salud pública y la reorganización propuesta de las agencias federales probablemente perjudiquen este avance, según un nuevo informe.
El informe Pain in the Nation 2025: the Epidemics of Alcohol, Drug, and Suicide Deaths (Dolor en el país 2025: la epidemia de muertes por alcohol, drogas y suicidio), que hoy publica Trust for America’s Health, expone que la cantidad conjunta de decesos a causa del alcohol, las drogas y los suicidios en los Estados Unidos disminuyeron en 2023 por segundo año consecutivo, tras dos décadas en las cuales tales decesos aumentaban a un ritmo alarmante. Aun así, más de 200.000 estadounidenses murieron a causa de sobredosis por alcohol, drogas o suicidio en 2023, el doble de la tasa por tales causas de muerte de hace 20 años atrás.
Estos nuevos datos ponen de manifiesto el valor de la inversión en salud mental y en los programas de prevención de consumo de sustancias como, por ejemplo, garantizar el acceso a los servicios correspondientes de salud mental, trastorno por consumo de sustancias e intervención por crisis, acceso a medicamentos que revierten la sobredosis, y la inversión en la salud mental y la resiliencia de los niños. No obstante, en los datos también se observa que se necesita hacer mucho más para garantizar que el avance contra las muertes a causa del alcohol, las drogas y el suicidio se mantengan, además de que las disminuciones logradas respecto a tales decesos están produciéndose en cada una de las comunidades y entre todos los grupos poblacionales.
“Los datos demuestran que en las décadas de inversión y desarrollo de capacidades con respecto a la prevención del consumo de sustancias, los programas de reducción de riesgos y los servicios de salud mental ayudaron a disminuir las muertes relacionadas con este flagelo. Actualmente, el desafío consiste en basarse en estas inversiones y mantener este avance. Con estos programas se salvan vidas, y no se debería recortar su financiamiento”, declaró Nadine Gracia, M.D., MSCE, presidenta y directora general de Trust for America’s Health.
Las tasas de sobredosis por drogas disminuyen, pero aún estamos en niveles trágicos.
En 2023, 105.007 estadounidenses en todo el país murieron a causa de sobredosis por drogas. Tras los aumentos precipitados en la tasa de muertes por sobredosis en 2020 y en 2021, la tasa general de mortalidad por sobredosis en 2022 no se modificó prácticamente y la tasa de mortalidad en 2023 fue un 4 por ciento menor. Los datos de mortalidad provisorios durante 2024 indican una disminución sin precedentes en un año del 27 por ciento en las muertes por sobredosis a nivel nacional. Se observaron en siete estados (Luisiana, Michigan, New Hampshire, Ohio, Virginia, West Virginia, y Wisconsin) y en Washington D.C. las disminuciones más importantes al tener bajas del 35 por ciento o más en muertes por sobredosis durante el año.
Según expertos en salud pública, los sistemas de datos mejorados que permiten hacer un seguimiento en tiempo real del consumo de sustancias y sus efectos, la ampliación y la eficacia de estrategias de prevención de sobredosis como los programas que garantizan el acceso a la naloxona y a la buprenorfina, o herramientas de control de drogas, tuvieron en conjunto un papel importante en la baja de las tasas de mortalidad.
No obstante, la mejora no fue uniforme en todos los grupos poblacionales ni regiones del país. En 2023, la población blanca fue el único grupo poblacional que tuvo una disminución estadísticamente significativa con respecto a las muertes por sobredosis de drogas; otros grupos poblacionales tuvieron cambios poco significativos o aumentos. Las tasas de muerte por sobredosis de drogas en 2023 fueron las más altas en los grupos poblacionales indoamericano y nativos de Alaska (AI/AN) (65 muertes por cada 100.000 habitantes), en adultos de 35 a 54 años (57,3 muertes por cada 100.000 habitantes), en la población de color (48,5 muertes por cada 100.000 habitantes), y en los hombres (45,6 muertes por cada 100.000 habitantes).
Disminución de las muertes inducidas por el alcohol
En 2023, 47.938 estadounidenses murieron por causas inducidas por el alcohol. La tasa general de mortalidad inducida por el alcohol ajustada por edad disminuyó en un 7 por ciento de 2022 a 2023 (de 13,5 a 12,6 muertes por cada 100.000 habitantes). Esta reducción se acumuló a un 6 por ciento de disminución del año anterior y atravesó a casi todos los grupos demográficos y geográficos, aunque dichas muertes aún afectan de manera desproporcionada a determinados grupos. Las tasas de muerte inducidas por el alcohol en 2023 fueron las más altas en los grupos poblacionales IA/NA (61,5 muertes por cada 100.000 habitantes), en adultos de 55 a 74 años (32,5 muertes por cada 100.000 habitantes), en adultos de 35 a 54 años (20,2 muertes por cada 100.000 habitantes), y en los hombres (18,1 muertes por cada 100.000 habitantes).
Sin cambios en las muertes por suicidio
La tasa de mortalidad general por suicidio en los Estados Unidos sigue prácticamente igual de 2022 a 2023 (14,2 y 14,1 muertes por cada 100.000 habitantes, respectivamente). En 2023, 49.316 estadounidenses murieron por causas del suicidio. Las tasas de muerte por suicidio ajustada por edad en 2023 fueron las más altas en los grupos poblacionales AI/AN (23,8 muertes por cada 100.000 habitantes), en los hombres (22,7 muertes por cada 100.000 habitantes), y en los adultos de 75 años o más (20,3 muertes por cada 100.000 habitantes).
La cancelación de presupuestos y los recortes futuros en los programas de prevención costarán vidas
Si bien con estos datos se demuestran avances reales, la comunidad de la salud pública se encuentra unida en esta preocupación con respecto a los cambios en los avances debido a los recortes en la inversión federal relacionados con la promoción de la salud, la intervención en situaciones de crisis y los programas de prevención de sobredosis. Por ejemplo, el personal y la financiación del Centro de Lesiones de los CDC sufrieron una reducción drástica y se ha propuesto eliminar al Centro en la solicitud de presupuesto del gobierno para el año fiscal 2026. El Centro de Lesiones lleva a cabo investigaciones y recopila datos. Aproximadamente, el 80 por ciento de su financiación se destina a los estados y demás entidades para la prevención de sobredosis, suicidios y experiencias infantiles negativas (ACE).
Asimismo, la Administración de Servicios de Salud Mental y Abuso de Sustancias (SAMHSA) ha sufrido importantes reducciones en su dotación de personal, lo que incluyó personal que trabajaba en la Línea 988 de atención al suicidio y situaciones de crisis y un potencial recorte de presupuesto de 1,07 mil millones para el año fiscal 2026. El gobierno propuso incorporar a los programas que queden de la SAMHSA y del Centro de Lesiones en la nueva Administración para unos Estados Unidos Saludables. Estas acciones siguieron a la recuperación del gobierno de miles de millones de dólares de financiación a la salud pública que ya estaban en marcha en los estado y comunidades de todo el país, incluida la prevención del suicidio.
En el informe Pain in the Nation, se llama a una inversión constante en los programas de prevención y reducción de riesgos y se incluyen recomendaciones sobre medidas que los representantes políticos a nivel federal y estatal deberían tomar, entre las que se incluyen:
- Proteger y apoyar las inversiones en los sistemas de salud pública y conductual y en programas de prevención de lesiones y violencia a fin de mejorar la salud mental y el bienestar de todos los ciudadanos de los Estados Unidos;
- Seguir mejorando los sistemas de datos, como Datos de sobredosis para la acción de los CDC, para hacer el seguimiento de las tendencias emergentes según las métricas geográficas, demográficas y por tipo de droga con el fin de orientar las respuestas a nivel local, estatal y nacional y prevenir casos de sobredosis y muertes en tiempo real;
- Enfocarse en las causas subyacentes de los trastornos por consumo de sustancias por medio de la intervención temprana y políticas de prevención incluidos los programas de ampliación de resiliencia y prevención de consumo de sustancias en las escuelas y aumento del acceso a servicios sociales y de salud mental para los niños y sus familias;
- Maximizar las estrategias de reducción de riesgos y los tratamientos de trastornos por consumo de sustancias a fin de disminuir el riesgo de sobredosis, y dar apoyo a las iniciativas para limitar el acceso a medios fatales de suicidio;
- Respaldar la continuidad de los programas de intervención de crisis y ampliar la dotación de personal para que brinde tratamiento de salud mental y por consumo de sustancias; Desarrollar la capacidad en la comunidad para garantizar el acceso a los servicios de salud mental y consumo de sustancias para todos los que necesiten estos servicios.
Lea el informe completo en: https://www.tfah.org/report-details/pain-in-the-nation-2025/
Trust for America’s Health es una organización sin fines de lucro no partidaria relacionada con políticas, investigación y defensa de la salud pública que fomenta la salud óptima para cada una de las personas y comunidades, y prioriza la prevención de enfermedades y lesiones a nivel nacional. Trust for America’s Health (tfah.org)
Pain in the Nation 2025: The Epidemics of Alcohol, Drug, and Suicide Deaths
2024 Year in Review and Looking Ahead to 2025
During 2024, Trust for America’s Health (TFAH) continued its work to create a more resilient, trusted, and equitable public health system, and a healthier nation.
TFAH continued its work in a number of critical issue areas to improve the nation’s health, including emergency preparedness, public health funding, chronic disease prevention, the role of food and nutrition policy in stemming the nation’s obesity crisis, preventing substance misuse and suicide, supporting healthy aging, and addressing the health impacts of climate change and other environmental health risks.
Progress and Risks
The nation’s public health system is at an inflection point; progress has been made in many areas but there are also continuing and potential new risks to the nation’s health. The following are examples of areas of progress and areas of risk.
Areas of progress:
- Drug overdose deaths, including from fentanyl, are down. The reduction can be credited in part to the increased availability of treatment options and the adoption of harm reduction strategies such as readily available naloxone, the overdose reversal drug, in many communities. However, disparities persist, with overdose rates increasing in many Black and Native American communities.
- COVID-19 infection rates are currently low across the country, a testament to what can be achieved when the public health community rallies and has the funding and resources necessary to meet an immediate challenge.
- Investments in public health data modernization, wastewater surveillance, and the Centers for Disease Control and Prevention’s (CDC) Center for Forecasting and Outbreak Analytics have improved the nation’s ability to identify and track emerging health threats. The Center has awarded more than $100 million to partners who are technologically advancing the use of outbreak data to control infectious disease spread.
- Fifty-nine state and local health departments have earned Age-Friendly Public Health Systems Recognition Status through TFAH’s Age-Friendly Public Health Systems initiative by making healthy aging a core function of the department. In addition, four public health organizations and 154 individual public health practitioners have been recognized as public health champions.
- Fifteen states and D.C. have adopted paid sick leave laws which require private employers to provide paid sick leave to employees attending to their own or a family member’s health. Alaska, Missouri, and Nebraska will require employers to provide paid sick leave beginning in 2025. Paid sick leave has been a long-standing TFAH policy recommendation.
Areas of risk:
- Public health faces a serious funding cliff as monies infused into the public health system as part of the pandemic response are expiring or in some cases rescinded. The loss of such funding returns the public health system to the state of underfunding it experienced for decades prior to the global pandemic. TFAH’s annual report, The Impact of Chronic Underfunding on America’s Public Health System 2024: Trends, Risks, and Recommendations called attention to the critical need to increase investment in public health on a sustained basis.
- The COVID-19 pandemic exposed serious gaps in the nation’s emergency infrastructure that have not been fully addressed. Furthermore, misinformation about the pandemic, particularly about lifesaving COVID-19 vaccines, contributed to an uptick in mistrust of public health officials that could lead to more vaccine hesitancy and challenges to important public health authorities, all of which could make containing future disease outbreaks more difficult.
- New disease outbreaks such as the H5N1 Bird Flu could grow.
- Rates of recommended childhood vaccinations are down.
- Health disparities continue to impact the nation. Rates of chronic disease are on the rise in every community but are higher, for example, among many communities of color and in rural communities, due to structural barriers to health like access to healthy and affordable food, secure housing, and opportunities for physical activity in those communities.
- Health risks are also increasing due to an increase in the number and severity of weather-related incidents including extended periods of extreme heat and extreme heat in regions of the country unaccustomed to such weather.
Working With Partners and Providing Leadership to Strengthen the Nation’s Public Health Ecosystem
TFAH released its Pathway to a Healthier America: A Blueprint for Strengthening Public Health for the Next Administration and Congress in October, after consultation with more than 45 experts, practitioners, organizations, and community members. The Blueprint provides the incoming Administration and Congress a policy roadmap for improving the nation’s health, economy, and national security within six priority areas: 1) invest in public health infrastructure and workforce, 2) strengthen prevention, readiness, and response to health security threats, 3) promote the health and well-being of individuals, families, and communities across the lifespan, 4) advance health equity by addressing structural discrimination, 5) address the non-medical drivers of health to improve the nation’s health outcomes, and 6) enhance and protect the scientific integrity, effectiveness, and accountability of agencies charged with protecting the health of all Americans.
Working with partners across multiple sectors is central to TFAH’s work. TFAH staff led or participated in a number of coalitions during 2024, including the Coalition for Health Funding, the CDC Coalition, the Common Health Coalition, the Well-Being Working Group, the Injury and Violence Prevention Network, National Alliance for Nutrition and Activity, the Coalition to Stop Flu, the Adult Vaccine Access Coalition, the Age-Friendly Ecosystem Collaborative, the National Alliance to Impact the Social Determinants of Health, the National Commission on Climate and Workforce Health, and the National Council on Environmental Health & Equity.
Advocating for Evidence-Based Solutions
A healthy community supports the health of individuals and families by creating access to non-medical drivers of health such as secure housing, transportation, quality healthcare, high-quality childcare and educational opportunities, and jobs that pay a living wage. Such health security supports individuals, families, communities, and the nation’s economy.
Throughout the year, TFAH convened partners to strategize ways to effectively advance health promoting policies and programs at the federal and state levels. In addition, TFAH staff worked with numerous federal agencies and offices, like CDC, FDA, and SAMHSA, as well as public health organizations such as the Association of State and Territorial Health Officials (ASTHO), the National Association of County and City Health Officials (NACCHO), Big Cities Health Coalition, and the National Governors Association to advance policies and garner support for programs that will improve Americans’ health. Among TFAH’s legislative goals for 2024 and moving into 2025 are increased and sustained investment in public health agencies, infrastructure, and programs; passage of a new Farm bill that provides access to nutrition support programs; reauthorization of the Pandemic and All Hazards Preparedness Act and the Older Americans Act; and passage of the Public Health Infrastructure Saves Lives Act and the Social Determinants of Health Act.
These advocacy efforts earned numerous policy wins, including the U.S. Department of Agriculture’s (USDA) updates to school meals formulas and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) benefit food packages that aligns with TFAH recommendations.
TFAH’s core annual reports, which track data and recommend policy solutions in the areas of emergency preparedness, public health funding, preventing substance misuse and suicide, and addressing the nation’s obesity crisis, continue to be a critical source for data trends and evidence-based policy and program solutions for health officials, policymakers, other decision-makers, and advocates across the country.
Making Healthy Aging a Core Function of Local Health Departments
Through its Age-Friendly Public Health Systems Initiative (AFPHS), TFAH continues to provide guidance and resources to state and local health departments to help them promote healthy aging in their communities. During 2024, AFPHS co-hosted the 2024 National Healthy Aging Symposium with the U.S. Department of Health and Human Services’ (HHS) Office of Disease Prevention and Health Promotion. The symposium brought together speakers from sectors across all levels of government, philanthropy, academia, nonprofits, community-based organizations, tribal representatives, and others who shared their perspectives on important topics related to healthy aging including caregiving, brain health, the caregiving workforce, transportation, housing, and social engagement. TFAH also launched the Age-Friendly Ecosystem Collaborative to continuously engage organizations and sectors central to healthy aging.
Supporting Public Health Communicators
TFAH continues to be a managing partner of the Public Health Communications Collaborative (PHCC). PHCC provides no-cost messaging resources and communications training to state and local health departments to help the field effectively address the public’s information needs on public health issues. The Collaborative was first established during the COVID-19 pandemic and now works across the public health sector on such issues as H5N1 Bird Flu, Mpox, protecting health during periods of extreme heat, and vaccine confidence. Its training materials include resources on strengthening public health through community engagement, responding to misinformation, and using social media in health communications. The PHCC newsletter is shared with over 38,000 opted-in subscribers, and its website has earned over 1.2 million page views since its launch in 2020.
Looking Ahead
The 2025 calendar year promises to be pivotal for the nation’s health. TFAH looks forward to bringing evidence-based policy recommendations to the new Administration and Congress, particularly on issues such as emergency preparedness, chronic disease prevention, mental health, veterans’ and rural health, and investing in prevention to reverse the pattern of increasing healthcare spending without better health outcomes. We are committed to making the case for policies and programs that address the non-medical drivers of health in order to promote the nation’s health and economic security.
Over 50 Public Health Advocacy Organizations Support Robust Investment in CDC Suicide Prevention
(November 1, 2024 – Washington, DC) – According to data from the Centers for Disease Control and Prevention (CDC), the number of suicides increased in 2022 to historic peak levels—over 49,000 deaths—after slight declines in 2019 and 2020. Suicide is the second leading cause of death among Americans between the ages of 10-14 and 25-34, and suicide rates increased by 36 percent between 2000 and 2021. The complex nature of suicide requires a comprehensive approach to prevention that focuses on disproportionately affected populations, uses data to understand risk factors associated with suicide in these groups, and applies the best available evidence to decrease risk and increase protective factors.
In a recent letter to key Congressional leaders, TFAH and the American Foundation for Suicide Prevention (AFSP) led more than 50 public health advocacy organizations in urging increased investment in these approaches through the CDC Comprehensive Suicide Prevention Program (CSP). Established in 2020, the CSP currently funds 24 initiatives nationwide through cooperative agreements designed to implement and evaluate a comprehensive public health approach to suicide prevention, with a special focus on populations that are disproportionately affected by suicide. These CSP initiatives have led to significant benefits, including decreases in suicide rates and increased training, awareness, and data collection. For example, the veteran and servicemember population that CSP initiatives served saw a 6.5% reduction in suicide rates from 2019-2021.
As the letter explains, “[b]y promoting mental health awareness, encouraging early intervention, and supporting individuals in crisis, the CSP plays a pivotal role in addressing one of the most serious public health challenges of our time.” TFAH and AFSP urge Congressional leaders to provide robust funding for the CSP to save lives and foster hope for Americans in crisis.



