¿Cómo se puede mantener y ampliar el avance para todas las comunidades?
(Washington, D.C., 28 de mayo de 2025). Las muertes a causa de sobredosis por drogas y abuso de alcohol disminuyeron en los Estados Unidos en 2023, según datos de los Centros para el control y prevención de enfermedades (CDC) y de los últimos datos provisorios publicados por los CDC en 2024, en donde que estima una baja sin precedentes del 27 % en un año en las muertes por sobredosis. Estas disminuciones son alentadoras y probablemente se relacionaron con una serie de factores, entre los que se incluyen las inversiones en prevención primaria, la salud mental, la reducción de riesgos y los programas de prevención de sobredosis. No obstante, los recortes presupuestarios actuales y propuestos a nivel federal, la reducción de la fuerza laboral de la salud pública y la reorganización propuesta de las agencias federales probablemente perjudiquen este avance, según un nuevo informe.
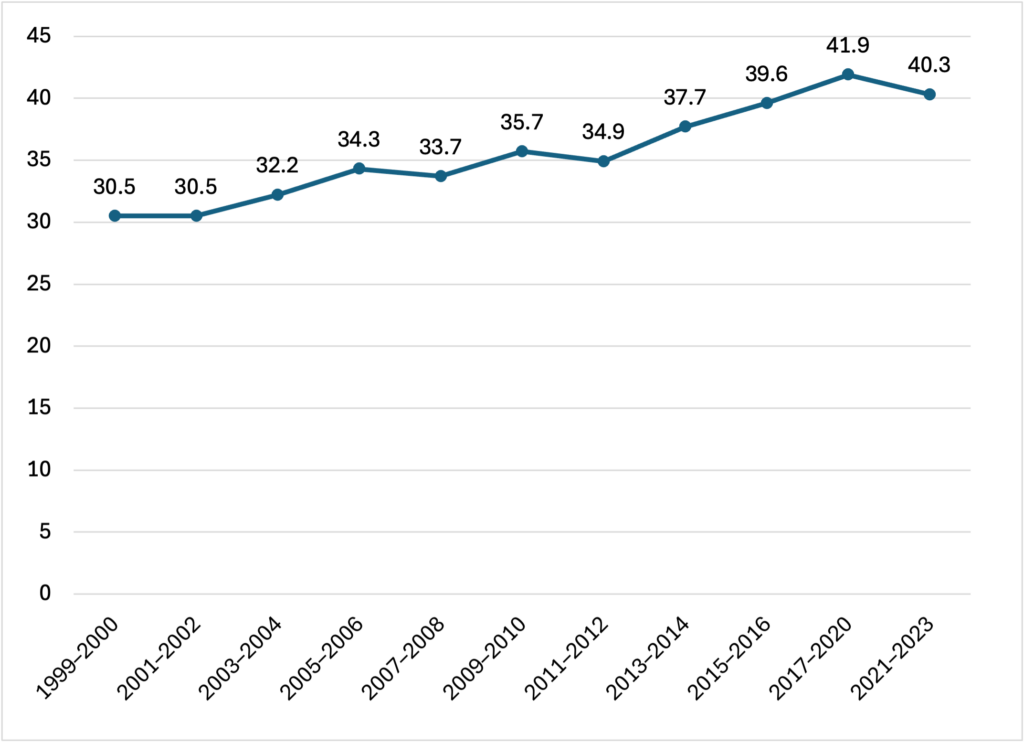
El informe Pain in the Nation 2025: the Epidemics of Alcohol, Drug, and Suicide Deaths (Dolor en el país 2025: la epidemia de muertes por alcohol, drogas y suicidio), que hoy publica Trust for America’s Health, expone que la cantidad conjunta de decesos a causa del alcohol, las drogas y los suicidios en los Estados Unidos disminuyeron en 2023 por segundo año consecutivo, tras dos décadas en las cuales tales decesos aumentaban a un ritmo alarmante. Aun así, más de 200.000 estadounidenses murieron a causa de sobredosis por alcohol, drogas o suicidio en 2023, el doble de la tasa por tales causas de muerte de hace 20 años atrás.
Estos nuevos datos ponen de manifiesto el valor de la inversión en salud mental y en los programas de prevención de consumo de sustancias como, por ejemplo, garantizar el acceso a los servicios correspondientes de salud mental, trastorno por consumo de sustancias e intervención por crisis, acceso a medicamentos que revierten la sobredosis, y la inversión en la salud mental y la resiliencia de los niños. No obstante, en los datos también se observa que se necesita hacer mucho más para garantizar que el avance contra las muertes a causa del alcohol, las drogas y el suicidio se mantengan, además de que las disminuciones logradas respecto a tales decesos están produciéndose en cada una de las comunidades y entre todos los grupos poblacionales.
“Los datos demuestran que en las décadas de inversión y desarrollo de capacidades con respecto a la prevención del consumo de sustancias, los programas de reducción de riesgos y los servicios de salud mental ayudaron a disminuir las muertes relacionadas con este flagelo. Actualmente, el desafío consiste en basarse en estas inversiones y mantener este avance. Con estos programas se salvan vidas, y no se debería recortar su financiamiento”, declaró Nadine Gracia, M.D., MSCE, presidenta y directora general de Trust for America’s Health.
Las tasas de sobredosis por drogas disminuyen, pero aún estamos en niveles trágicos.
En 2023, 105.007 estadounidenses en todo el país murieron a causa de sobredosis por drogas. Tras los aumentos precipitados en la tasa de muertes por sobredosis en 2020 y en 2021, la tasa general de mortalidad por sobredosis en 2022 no se modificó prácticamente y la tasa de mortalidad en 2023 fue un 4 por ciento menor. Los datos de mortalidad provisorios durante 2024 indican una disminución sin precedentes en un año del 27 por ciento en las muertes por sobredosis a nivel nacional. Se observaron en siete estados (Luisiana, Michigan, New Hampshire, Ohio, Virginia, West Virginia, y Wisconsin) y en Washington D.C. las disminuciones más importantes al tener bajas del 35 por ciento o más en muertes por sobredosis durante el año.
Según expertos en salud pública, los sistemas de datos mejorados que permiten hacer un seguimiento en tiempo real del consumo de sustancias y sus efectos, la ampliación y la eficacia de estrategias de prevención de sobredosis como los programas que garantizan el acceso a la naloxona y a la buprenorfina, o herramientas de control de drogas, tuvieron en conjunto un papel importante en la baja de las tasas de mortalidad.
No obstante, la mejora no fue uniforme en todos los grupos poblacionales ni regiones del país. En 2023, la población blanca fue el único grupo poblacional que tuvo una disminución estadísticamente significativa con respecto a las muertes por sobredosis de drogas; otros grupos poblacionales tuvieron cambios poco significativos o aumentos. Las tasas de muerte por sobredosis de drogas en 2023 fueron las más altas en los grupos poblacionales indoamericano y nativos de Alaska (AI/AN) (65 muertes por cada 100.000 habitantes), en adultos de 35 a 54 años (57,3 muertes por cada 100.000 habitantes), en la población de color (48,5 muertes por cada 100.000 habitantes), y en los hombres (45,6 muertes por cada 100.000 habitantes).
Disminución de las muertes inducidas por el alcohol
En 2023, 47.938 estadounidenses murieron por causas inducidas por el alcohol. La tasa general de mortalidad inducida por el alcohol ajustada por edad disminuyó en un 7 por ciento de 2022 a 2023 (de 13,5 a 12,6 muertes por cada 100.000 habitantes). Esta reducción se acumuló a un 6 por ciento de disminución del año anterior y atravesó a casi todos los grupos demográficos y geográficos, aunque dichas muertes aún afectan de manera desproporcionada a determinados grupos. Las tasas de muerte inducidas por el alcohol en 2023 fueron las más altas en los grupos poblacionales IA/NA (61,5 muertes por cada 100.000 habitantes), en adultos de 55 a 74 años (32,5 muertes por cada 100.000 habitantes), en adultos de 35 a 54 años (20,2 muertes por cada 100.000 habitantes), y en los hombres (18,1 muertes por cada 100.000 habitantes).
Sin cambios en las muertes por suicidio
La tasa de mortalidad general por suicidio en los Estados Unidos sigue prácticamente igual de 2022 a 2023 (14,2 y 14,1 muertes por cada 100.000 habitantes, respectivamente). En 2023, 49.316 estadounidenses murieron por causas del suicidio. Las tasas de muerte por suicidio ajustada por edad en 2023 fueron las más altas en los grupos poblacionales AI/AN (23,8 muertes por cada 100.000 habitantes), en los hombres (22,7 muertes por cada 100.000 habitantes), y en los adultos de 75 años o más (20,3 muertes por cada 100.000 habitantes).
La cancelación de presupuestos y los recortes futuros en los programas de prevención costarán vidas
Si bien con estos datos se demuestran avances reales, la comunidad de la salud pública se encuentra unida en esta preocupación con respecto a los cambios en los avances debido a los recortes en la inversión federal relacionados con la promoción de la salud, la intervención en situaciones de crisis y los programas de prevención de sobredosis. Por ejemplo, el personal y la financiación del Centro de Lesiones de los CDC sufrieron una reducción drástica y se ha propuesto eliminar al Centro en la solicitud de presupuesto del gobierno para el año fiscal 2026. El Centro de Lesiones lleva a cabo investigaciones y recopila datos. Aproximadamente, el 80 por ciento de su financiación se destina a los estados y demás entidades para la prevención de sobredosis, suicidios y experiencias infantiles negativas (ACE).
Asimismo, la Administración de Servicios de Salud Mental y Abuso de Sustancias (SAMHSA) ha sufrido importantes reducciones en su dotación de personal, lo que incluyó personal que trabajaba en la Línea 988 de atención al suicidio y situaciones de crisis y un potencial recorte de presupuesto de 1,07 mil millones para el año fiscal 2026. El gobierno propuso incorporar a los programas que queden de la SAMHSA y del Centro de Lesiones en la nueva Administración para unos Estados Unidos Saludables. Estas acciones siguieron a la recuperación del gobierno de miles de millones de dólares de financiación a la salud pública que ya estaban en marcha en los estado y comunidades de todo el país, incluida la prevención del suicidio.
En el informe Pain in the Nation, se llama a una inversión constante en los programas de prevención y reducción de riesgos y se incluyen recomendaciones sobre medidas que los representantes políticos a nivel federal y estatal deberían tomar, entre las que se incluyen:
- Proteger y apoyar las inversiones en los sistemas de salud pública y conductual y en programas de prevención de lesiones y violencia a fin de mejorar la salud mental y el bienestar de todos los ciudadanos de los Estados Unidos;
- Seguir mejorando los sistemas de datos, como Datos de sobredosis para la acción de los CDC, para hacer el seguimiento de las tendencias emergentes según las métricas geográficas, demográficas y por tipo de droga con el fin de orientar las respuestas a nivel local, estatal y nacional y prevenir casos de sobredosis y muertes en tiempo real;
- Enfocarse en las causas subyacentes de los trastornos por consumo de sustancias por medio de la intervención temprana y políticas de prevención incluidos los programas de ampliación de resiliencia y prevención de consumo de sustancias en las escuelas y aumento del acceso a servicios sociales y de salud mental para los niños y sus familias;
- Maximizar las estrategias de reducción de riesgos y los tratamientos de trastornos por consumo de sustancias a fin de disminuir el riesgo de sobredosis, y dar apoyo a las iniciativas para limitar el acceso a medios fatales de suicidio;
- Respaldar la continuidad de los programas de intervención de crisis y ampliar la dotación de personal para que brinde tratamiento de salud mental y por consumo de sustancias; Desarrollar la capacidad en la comunidad para garantizar el acceso a los servicios de salud mental y consumo de sustancias para todos los que necesiten estos servicios.
Lea el informe completo en: https://www.tfah.org/report-details/pain-in-the-nation-2025/
Trust for America’s Health es una organización sin fines de lucro no partidaria relacionada con políticas, investigación y defensa de la salud pública que fomenta la salud óptima para cada una de las personas y comunidades, y prioriza la prevención de enfermedades y lesiones a nivel nacional. Trust for America’s Health (tfah.org)