During 2024, Trust for America’s Health (TFAH) continued its work to create a more resilient, trusted, and equitable public health system, and a healthier nation.
TFAH continued its work in a number of critical issue areas to improve the nation’s health, including emergency preparedness, public health funding, chronic disease prevention, the role of food and nutrition policy in stemming the nation’s obesity crisis, preventing substance misuse and suicide, supporting healthy aging, and addressing the health impacts of climate change and other environmental health risks.
Progress and Risks
The nation’s public health system is at an inflection point; progress has been made in many areas but there are also continuing and potential new risks to the nation’s health. The following are examples of areas of progress and areas of risk.
Areas of progress:
- Drug overdose deaths, including from fentanyl, are down. The reduction can be credited in part to the increased availability of treatment options and the adoption of harm reduction strategies such as readily available naloxone, the overdose reversal drug, in many communities. However, disparities persist, with overdose rates increasing in many Black and Native American communities.
- COVID-19 infection rates are currently low across the country, a testament to what can be achieved when the public health community rallies and has the funding and resources necessary to meet an immediate challenge.
- Investments in public health data modernization, wastewater surveillance, and the Centers for Disease Control and Prevention’s (CDC) Center for Forecasting and Outbreak Analytics have improved the nation’s ability to identify and track emerging health threats. The Center has awarded more than $100 million to partners who are technologically advancing the use of outbreak data to control infectious disease spread.
- Fifty-nine state and local health departments have earned Age-Friendly Public Health Systems Recognition Status through TFAH’s Age-Friendly Public Health Systems initiative by making healthy aging a core function of the department. In addition, four public health organizations and 154 individual public health practitioners have been recognized as public health champions.
- Fifteen states and D.C. have adopted paid sick leave laws which require private employers to provide paid sick leave to employees attending to their own or a family member’s health. Alaska, Missouri, and Nebraska will require employers to provide paid sick leave beginning in 2025. Paid sick leave has been a long-standing TFAH policy recommendation.
Areas of risk:
- Public health faces a serious funding cliff as monies infused into the public health system as part of the pandemic response are expiring or in some cases rescinded. The loss of such funding returns the public health system to the state of underfunding it experienced for decades prior to the global pandemic. TFAH’s annual report, The Impact of Chronic Underfunding on America’s Public Health System 2024: Trends, Risks, and Recommendations called attention to the critical need to increase investment in public health on a sustained basis.
- The COVID-19 pandemic exposed serious gaps in the nation’s emergency infrastructure that have not been fully addressed. Furthermore, misinformation about the pandemic, particularly about lifesaving COVID-19 vaccines, contributed to an uptick in mistrust of public health officials that could lead to more vaccine hesitancy and challenges to important public health authorities, all of which could make containing future disease outbreaks more difficult.
- New disease outbreaks such as the H5N1 Bird Flu could grow.
- Rates of recommended childhood vaccinations are down.
- Health disparities continue to impact the nation. Rates of chronic disease are on the rise in every community but are higher, for example, among many communities of color and in rural communities, due to structural barriers to health like access to healthy and affordable food, secure housing, and opportunities for physical activity in those communities.
- Health risks are also increasing due to an increase in the number and severity of weather-related incidents including extended periods of extreme heat and extreme heat in regions of the country unaccustomed to such weather.
Working With Partners and Providing Leadership to Strengthen the Nation’s Public Health Ecosystem
TFAH released its Pathway to a Healthier America: A Blueprint for Strengthening Public Health for the Next Administration and Congress in October, after consultation with more than 45 experts, practitioners, organizations, and community members. The Blueprint provides the incoming Administration and Congress a policy roadmap for improving the nation’s health, economy, and national security within six priority areas: 1) invest in public health infrastructure and workforce, 2) strengthen prevention, readiness, and response to health security threats, 3) promote the health and well-being of individuals, families, and communities across the lifespan, 4) advance health equity by addressing structural discrimination, 5) address the non-medical drivers of health to improve the nation’s health outcomes, and 6) enhance and protect the scientific integrity, effectiveness, and accountability of agencies charged with protecting the health of all Americans.
Working with partners across multiple sectors is central to TFAH’s work. TFAH staff led or participated in a number of coalitions during 2024, including the Coalition for Health Funding, the CDC Coalition, the Common Health Coalition, the Well-Being Working Group, the Injury and Violence Prevention Network, National Alliance for Nutrition and Activity, the Coalition to Stop Flu, the Adult Vaccine Access Coalition, the Age-Friendly Ecosystem Collaborative, the National Alliance to Impact the Social Determinants of Health, the National Commission on Climate and Workforce Health, and the National Council on Environmental Health & Equity.
Advocating for Evidence-Based Solutions
A healthy community supports the health of individuals and families by creating access to non-medical drivers of health such as secure housing, transportation, quality healthcare, high-quality childcare and educational opportunities, and jobs that pay a living wage. Such health security supports individuals, families, communities, and the nation’s economy.
Throughout the year, TFAH convened partners to strategize ways to effectively advance health promoting policies and programs at the federal and state levels. In addition, TFAH staff worked with numerous federal agencies and offices, like CDC, FDA, and SAMHSA, as well as public health organizations such as the Association of State and Territorial Health Officials (ASTHO), the National Association of County and City Health Officials (NACCHO), Big Cities Health Coalition, and the National Governors Association to advance policies and garner support for programs that will improve Americans’ health. Among TFAH’s legislative goals for 2024 and moving into 2025 are increased and sustained investment in public health agencies, infrastructure, and programs; passage of a new Farm bill that provides access to nutrition support programs; reauthorization of the Pandemic and All Hazards Preparedness Act and the Older Americans Act; and passage of the Public Health Infrastructure Saves Lives Act and the Social Determinants of Health Act.
These advocacy efforts earned numerous policy wins, including the U.S. Department of Agriculture’s (USDA) updates to school meals formulas and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) benefit food packages that aligns with TFAH recommendations.
TFAH’s core annual reports, which track data and recommend policy solutions in the areas of emergency preparedness, public health funding, preventing substance misuse and suicide, and addressing the nation’s obesity crisis, continue to be a critical source for data trends and evidence-based policy and program solutions for health officials, policymakers, other decision-makers, and advocates across the country.
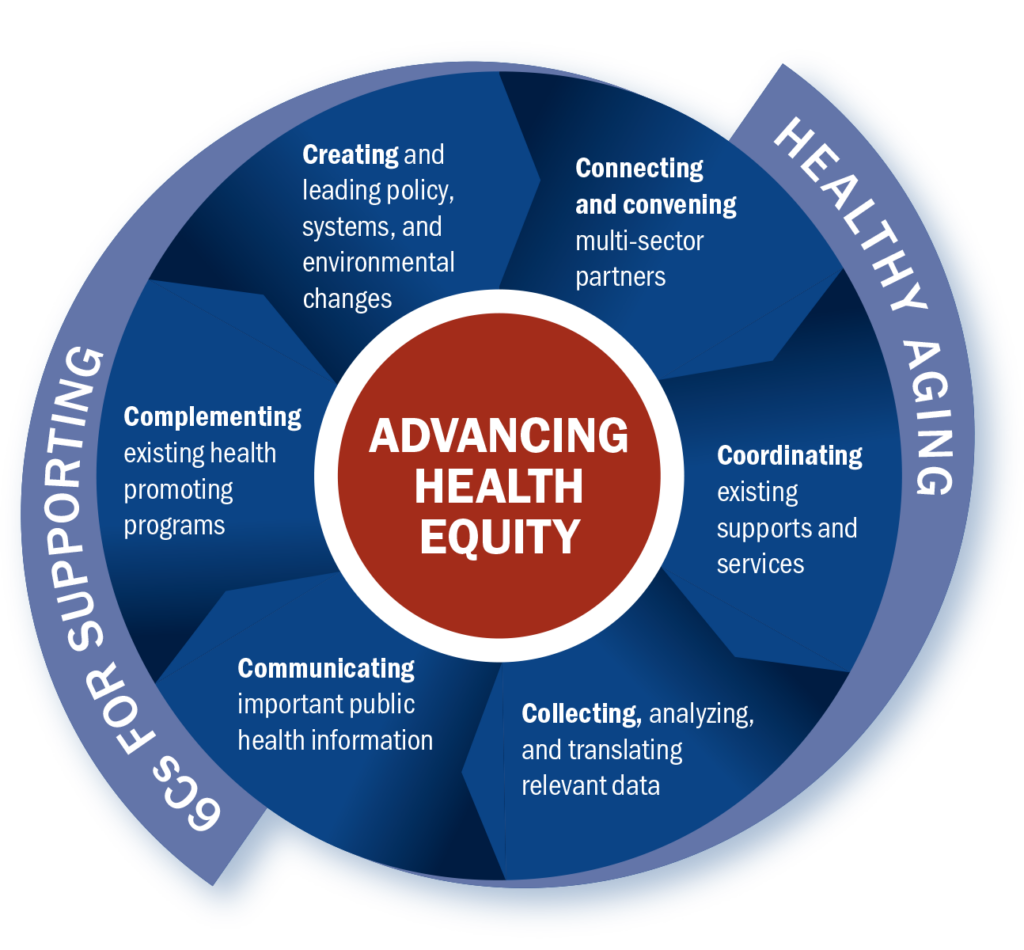
Making Healthy Aging a Core Function of Local Health Departments
Through its Age-Friendly Public Health Systems Initiative (AFPHS), TFAH continues to provide guidance and resources to state and local health departments to help them promote healthy aging in their communities. During 2024, AFPHS co-hosted the 2024 National Healthy Aging Symposium with the U.S. Department of Health and Human Services’ (HHS) Office of Disease Prevention and Health Promotion. The symposium brought together speakers from sectors across all levels of government, philanthropy, academia, nonprofits, community-based organizations, tribal representatives, and others who shared their perspectives on important topics related to healthy aging including caregiving, brain health, the caregiving workforce, transportation, housing, and social engagement. TFAH also launched the Age-Friendly Ecosystem Collaborative to continuously engage organizations and sectors central to healthy aging.
Supporting Public Health Communicators
TFAH continues to be a managing partner of the Public Health Communications Collaborative (PHCC). PHCC provides no-cost messaging resources and communications training to state and local health departments to help the field effectively address the public’s information needs on public health issues. The Collaborative was first established during the COVID-19 pandemic and now works across the public health sector on such issues as H5N1 Bird Flu, Mpox, protecting health during periods of extreme heat, and vaccine confidence. Its training materials include resources on strengthening public health through community engagement, responding to misinformation, and using social media in health communications. The PHCC newsletter is shared with over 38,000 opted-in subscribers, and its website has earned over 1.2 million page views since its launch in 2020.
Looking Ahead
The 2025 calendar year promises to be pivotal for the nation’s health. TFAH looks forward to bringing evidence-based policy recommendations to the new Administration and Congress, particularly on issues such as emergency preparedness, chronic disease prevention, mental health, veterans’ and rural health, and investing in prevention to reverse the pattern of increasing healthcare spending without better health outcomes. We are committed to making the case for policies and programs that address the non-medical drivers of health in order to promote the nation’s health and economic security.



 Megan: The Guide can be used by anyone who wants to build expertise in healthy aging, especially from a public health perspective. Our vision is that entire health department staffs will use it, but it’s also perfect for individuals or small teams to work through together.
Megan: The Guide can be used by anyone who wants to build expertise in healthy aging, especially from a public health perspective. Our vision is that entire health department staffs will use it, but it’s also perfect for individuals or small teams to work through together.




