Issue Category: Environmental Health
Comments to HUD on Proposed Immigration and Housing Rule ( July 2019)
Sign-on Letter to Congress in Support to CDC National Center for Environmental Health Fiscal Year 2020 Funding (February 2019)
Vaccines Prevent Infectious Disease Outbreaks and Protect Communities (August 2019)
Infectious diseases disrupt the lives millions of Americans every year. Fortunately, vaccines can prevent many of these diseases. Nonetheless, because the U.S. vaccination rates are lower than they should be, unnecessary illness and even death occurs.
For example, the seasonal flu causes much preventable suffering. The Centers for Disease Control and Prevention (CDC) found an estimated 80,000 people died—among them, 185 children—from seasonal flu in 2017–2018, nearly twice what is considered typical during an average flu year. In addition to the devastating health impacts, it is estimated that seasonal flu costs the nation approximately $87 billion in medical spending and lost work productivity annually.
The U.S. is currently in the midst of its worst measles outbreak in two decades, causing more than 1,000 cases. With the measles outbreak still growing, it is important to highlight the life-saving impacts of vaccines for people of all ages and take actions to ensure that vaccine use remains a common practice.
Key Findings
- Vaccines have helped save up to 3 million lives per year worldwide by preventing diseases such as hepatitis B, meningitis, measles and polio. Additionally, researchers say that every dollar spent on vaccination brings back return on investment in health, economic and societal benefits in 94 low to middle income countries.
- The CDC estimates that vaccination of children born between 1994 and 2018 in the U.S. will prevent 419 million illnesses, help avoid 936,000 deaths, and save nearly $1.9 trillion in total societal costs.
- In 2018, the CDC reported that the percentage of children under age 2 who had not received any recommended vaccinations quadrupled since 2001.
- Adult vaccination rates remain far below targets in Healthy People 2020, including for hepatitis B, seasonal flu, pneumococcal, and shingles.
- Seasonal flu vaccination rates for Americans ages 6 months and older dropped from 47 percent in the 2016-2017 season to 42 percent during the 2017-2018 season. The 2017– 2018 flu season in the United States was the deadliest in nearly 40 years—tragically underscoring the importance of annual vaccination.
- The World Health Organization has named vaccine hesitancy, the reluctance or refusal to vaccinate despite the availability of vaccines, as one of the top ten threats to global health.
Recommendations
- Significantly increase support for the vaccine infrastructure, outbreak prevention and response. CDC’s immunization program supports state and local immunization programs to increase vaccine rates among uninsured and underinsured adults and children, respond to outbreaks, educate the public and target hard-to-reach populations, improve vaccine confidence, establish partnerships, and improve information systems. Funding has not kept up with needs as states have to spend immunization dollars to respond to outbreaks, increases in the numbers of those who lack health insurance and vaccines, such as HPV, that are underused. Congress should significantly increase funding for CDC’s immunization program.
- Raise awareness about the importance of vaccination and improve vaccine acceptance. Government, healthcare providers, health systems and other trusted partners should use varied and targeted media channels to educate people about the importance, effectiveness, and safety of vaccinations. Congress should provide needed resources to the United States Department of Health and Human Services to study the causes for vaccine resistance and to educate clinical providers on methods for improving vaccine acceptance.
- Minimize vaccine exemptions for schoolchildren and healthcare workers. States should enact policies that enable universal childhood vaccinations to ensure children, their classmates, educators and the general public are protected from vaccine-preventable diseases. This includes eliminating non-medical exemptions and opposing legislation to expand exemptions. States should ensure medical vaccine exemptions are only given when appropriate and are not used as a de facto personal belief exemption in states where those exemptions have been eliminated. Healthcare personnel should also be required to receive all recommended vaccinations of the Advisory Committee on Immunization Practices (ACIP) in order to protect staff and patients, assure continuity of operations in the event of an outbreak and, achieve necessary healthcare infection control. Healthcare facilities should ensure access to vaccines for all staff and contractors and remove barriers for staff receiving vaccines.
- Ensure first-dollar coverage for recommended vaccines under Medicaid, Medicare, and commercial insurance. Public and private payers should ensure that ACIP-recommended vaccines are fully covered, as cost-sharing can be a significant barrier to vaccination.
- Increase the pool of providers who immunize. As new vaccines are approved, reaching target populations will be critical. States can expand certain health care providers’ roles and scopes of practice to increase the pool of professionals who give shots, such as pharmacists and paramedics. All insurance plans should consider including pharmacies and other complementary providers as in-network and receive equal payment for vaccine administration services for their adult and pediatric populations.
3 WINS Fitness: Free Exercise Classes get Communities Moving
Regular physical activity promotes good health and well-being. Yet, about 80 percent of American adults do not meet the minimum recommended levels for cardiovascular activity and strength training needed to support optimal health and prevent the risk of chronic diseases.
3 WINS Fitness seeks to improve community health by increasing people’s physical activity levels. Launched in 2011 as 100 Citizens by California State University, Northridge’s (CSUN) Department of Kinesiology in partnership with Recreation Park in San Fernando, CA, 3 WINS Fitness offers a tailored and comprehensive free exercise intervention that is sustainable and replicable through its delivery by university kinesiology students. Programs are provided at public parks, faith-based institutions, and public schools, and currently they operate at six sites across Los Angeles County serving over 300 participants.
In 2013 the White House recognized and gave an award to the program through First Lady Michelle Obama’s “Let’s Move!” campaign. Since then, the program has scaled to three other universities within the California State University system.
Their program’s “3 WINS” reflects their social impact priorities: community health, participant fitness, and student professional development.
WIN 1: Community Health
Access and affordability to safe places to engage in physical activity promotes optimal community health. However, many low-income communities do not have affordable access to safe places for physical activity, and thus have a disproportionate burden of disease compared to wealthier communities.
Steven Loy, Ph.D., professor of kinesiology at CSUN and founder/faculty advisor for 3 WINS Fitness says the program focuses on those underserved communities which are at high risk for diabetes, cardiovascular disease, obesity and other chronic diseases related to physical inactivity.
“Having a program in their neighborhood park, school, and church where they can easily walk to and exercise, especially where there are no other physical activity programs is important,” said Loy. “We are holding it in communities that county public health has identified as areas where health inequities exist, and we are helping to address the social determinants of health by improving the physical activity conditions of those communities.”
Loy says through their research with RAND Corporation and the data they have collected, they observed a greater use of park facilities with the introduction of structured physical activity, in particular for the senior population reflecting a sense of safety and community among themselves and their students.
WIN 2: Participant Health

3 WINS Fitness provides participants with a dynamic 60-minute exercise routine three times per week for adults of all ages and fitness abilities, including a falls prevention group, and free diabetes prevention program modified from the National Diabetes Prevention Program.
Loy noted, “participants who attend the three classes per week exceed the minimum recommended levels for cardiovascular activity and strength training cited in the 2018 Physical Activity Guidelines. Throughout the years, our 3 WINS Fitness participants have had many success stories.”
“Doctors said I would need surgery for a back injury, I was in constant pain, I couldn’t even lift my arms to brush my hair” said 3 WINS participant of two years Balvina Nuño. “Since joining 3 WINS, the injury has healed without surgery. I can now lift my arms over my head, and I have lost 30 pounds! I am thankful to God and the instructors for giving me my life back.”
Other participants of the program have also reported improved health.
“I started 3 WINS Fitness last summer and have lost over 40 pounds,” said Andrea Veronica. “I am diabetic and was required to inject insulin 6 times a day. Because of this program, today I am no longer required to inject myself or take any medication. I am happy and feel more energetic than ever!”
“I started this program in October 2017 as a pre-diabetic,” added Candy Lopez. “I have lost 24 pounds, and I feel happier and have more energy. I love coming here because the participants and instructors create such a strong family-like community that I feel motivated to come workout every time.”
WIN 3: Student Professional Development
The kinesiology students involved in the program include both undergraduate and graduate students trained and educated in exercise and human movement. For them, 3 WINS Fitness is an opportunity to apply their education, gain job-related experience, and grow in leadership skills and self-empowerment.
“Noting the constant changes happening in health care reform, I realized what we are doing through 3 WINS Fitness is so special and is soon, if not already, to become the face of preventative health care methods that is efficient, cost-effective, and helps not only me as a healthcare provider, but most importantly, the individuals in the communities around us attain their best level of health and fitness,” said Angelica Alberto, a former 3 WINS Fitness student volunteer who is now pursuing a Doctor of Physical Therapy and Master of Public Health dual degree at Northwestern University.
Loy says it is also an opportunity to show communities what those educated in kinesiology can do for public health.
“We have found that there are few opportunities created for kinesiology and public health to work together. We are trying to change that with upstream solutions to the ideas promoted by Public Health 3.0,” said Loy. “We have recruited students to create an ongoing army of individuals trained in physical activity who are pursuing additional public health education opportunities, and, are motivated and enthusiastic to deliver programming that reaches the whole community to improve health.”
Where is the Program Going?

3 WINS Fitness participants receive exercise programming from 3 WINS Fitness kinesiology students during a 3 WINS
Fitness Summit held in April 2018.
Throughout 3 WINS Fitness’ journey, partnerships have been critical. The program has teamed with public and private sector partnerships with parks and recreation, public health, universities and research institutions, hospitals, and health and fitness organizations to sustain, scale, and provide accessible physical activity programming to communities.
One of those partners is the American Council on Exercise (ACE). Cedric Bryant, Ph.D., ACE President and Chief Science Officer says “ACE’s partnership with 3 WINS Fitness helps us fulfill our mission to get people moving, regardless of age, gender, race, or socioeconomic background.”
In the spring of 2018, ACE partnered with 3 WIN Fitness to hold a Summit to demonstrate the program to stakeholders. One of the attendees included Loretta DiPietro, Ph.D., professor of exercise and nutrition sciences at the Milken Institute School of Public Health at George Washington University in Washington, D.C. She was also a committee member of the 2018 Physical Activity Guidelines Advisory Committee which reviewed the scientific evidence and prepared a report about physical activity and health for the second edition of the Physical Activity Guidelines for Americans.
She said, “I’ve been waiting my entire public health career to see the science of exercise and physical activity translated and scaled up to the community level so elegantly and effectively. The cultural wave of change in how communities adopt an active lifestyle begins now with 3WINS Fitness!”
According to a study done by the Centers for Disease Control and Prevention, 11.1 percent in total health care expenditures were associated with inadequate levels of physical activity. However, if programs were in place to help adults meet current guidelines for physical activity, the country could avert up to an estimated $117 billion in preventable health care spending.
Loy said 3 WINS Fitness is part of that solution, and their next goal is to scale 3 WINS Fitness through universities across the country by training staff to develop and sustain their own program specific to their community.
“There are over 700 universities with kinesiology programs,” said Loy. “Our experience in replicating our program, as well as scaling it to other universities has identified the challenges existing for collaboration among public health, kinesiology, parks and recreation, and faith-based organizations, but it has also been an 8-year demonstration that an affordable sustainable solution is possible if we work together. The university kinesiology model can drive community wide disease prevention programs which can be customized for the needs of the community.”
*3 WINS Fitness Banner Photo Credit: Carmen Anthony
Complete Streets Overview
TFAH Applauds Passage of Critical Preparedness Legislation
Adopting the Pandemic and All-Hazards Preparedness and Advancing Innovation Act Supports the Nation’s Health Security
(Washington, DC) – John Auerbach, president and CEO, of Trust for America’s Health (TFAH) today made the following statement regarding the congressional passage of the Pandemic and All-Hazards Preparedness and Advancing Innovation (PAHPAI) Act.
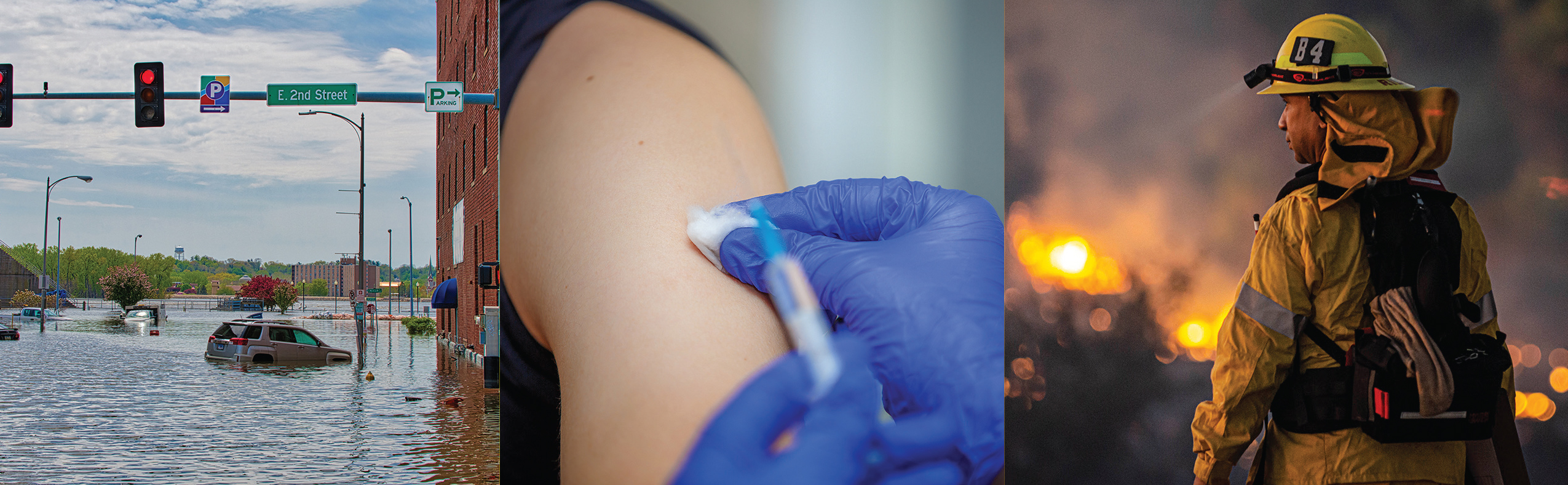
“Trust for America’s Health applauds Congress for working in a bipartisan manner to pass important legislation to advance our nation’s health security. The Pandemic and All-Hazards Preparedness and Advancing Innovation Act shows that we are learning the lessons from recent disasters and disease outbreaks and addressing ongoing challenges. Passage of this legislation, was a top recommendation in TFAH’s recent report, Ready or Not: Protecting the Public’s Health from Diseases, Disasters, and Bioterrorism.
During the Zika outbreak, it took about nine months to approve emergency supplemental funding. And recent severe weather showed that we are still not prepared for a worst-case scenario event. In this legislation, lawmakers try to address some of the gaps that these events exposed. The bill makes it easier to get money out more efficiently to address a public health emergency. It codifies the roles of federal agencies in managing important preparedness programs and ensures we are consistently improving the performance of awardees. It supports outbreak detection through workforce and strategy enhancements. It reauthorizes programs for research, development and stockpiling of medical countermeasures and seeks to speed the capability to deploy those products.
Public health and health care are at the frontlines in responding to health crises large and small. The fact that Congress passed this bill is acknowledgement that health security is national security.
Now, we call on Congress to give this legislation the teeth it needs by providing adequate funding for these critical public health programs.”
# # #
Trust for America’s Health is a nonprofit, nonpartisan organization that promotes optimal health for every person and community and makes the prevention of illness and injury a national priority. www.tfah.org. Twitter: @healthyamerica1
New TFAH Report: Persistent Underfunding of America’s Public Health System Makes the Nation Vulnerable and Puts Lives at Risk
Funding for public health programs via the CDC budget decreased by 10 percent over the last decade while public health risks grew
(Washington DC – April 24, 2019) – Chronic underfunding of the nation’s public health infrastructure has left the nation vulnerable to serious health and safety risks, according to a new report released today by Trust for America’s Health.
The report, The Impact of Chronic Underfunding on America’s Public Health System: Trends, Risks, and Recommendations, 2019, examines federal, state, and local public health funding trends and recommends needed investments and policy actions to prioritize prevention and effectively address 21st century health threats.
The federal government, primarily through the U.S. Centers for Disease Control and Prevention (CDC), provides critical support for the nation’s public health infrastructure including by funding a substantial portion of state and local public health programs. But, between Fiscal Year (FY) 2010 – Fiscal Year 2019, the CDC’s budget fell by 10 percent when adjusted for inflation. Cuts to the CDC budget have direct impacts on state and local public health departments’ budgets. In 2018, 17 states and the District of Columbia cut their public health spending.
“Our country is grappling with unprecedented public health problems including the opioid crisis, the increasing number of Americans with chronic diseases, virulent infectious diseases and a growing number of weather-related emergencies,” said John Auerbach, President and CEO of Trust for America’s Health. “The CDC budget is simply not sufficient to address these demands.”
“At a time when the country’s health security threats are increasing, reducing spending to prevent and respond to these risks is dangerous and makes Americans less safe,” Auerbach said.
“CDC funding represents the majority of public health funding nationally and locally. When CDC funding is cut, state and local governments are often forced to reduce funding for critical programs including those to prevent chronic and infectious diseases, to protect environmental health and to provide vaccinations for children, among many others. These are programs Americans need and support. They shouldn’t be constantly on the chopping-block,” Auerbach said.
Among the Report’s Key Findings Are:
- Over the past decade, the Centers for Disease Control and Prevention’s program funding—more than half of which goes to states, localities, and other nonfederal partners—decreased by 10 percent, after adjusting for inflation. At the same time, substance misuse has skyrocketed, the incidence of obesity and related health problems continue to climb, and the threat of weather-related emergencies is on the rise.
- Federal funding cuts negatively affect state health departments as these funds are a primary source of state public health budgets. On average, federal funding comprises 48 percent of state public health budgets. Similarly, these spending cuts have serious consequences for local health departments given that federal and state allocations constitute a substantial portion of local health departments’ budgets.
- Seventeen states and the District of Columbia cut their public health funding in FY 2018.
- One-fifth of local health departments reported decreases in their FY 2017 budgets.
- Multiple years of funding cuts contributed to more than 55,000 lost jobs at local health departments from 2008-17. These cuts undermine efforts to hire, train, and retain a strong public health workforce, which in turn limits governments’ ability to effectively protect and promote the health of their residents.
- Cuts to public health funding often result in higher health care costs as preventable illnesses and injuries are major causes of hospitalization and other medical interventions.
The Report’s Topline Recommendations Include:
- Increase federal investments in public health. To protect the health and safety of all the country’s residents we need more funding for public health programs, not less.
- Provide sufficient, full-year funding for federal agencies to avoid interruptions in funding for critical health security programs.
- Increase state and local investment in public health, prioritizing prevention and the social determinants of health.
- Work across sectors to improve the effectiveness and efficiency of public health investments.
- Ease coordination of funding from multiple sources.
# # #
Trust for America’s Health is a nonprofit, nonpartisan organization that promotes optimal health for every person and community and makes the prevention of illness and injury a national priority.
The Impact of Chronic Underfunding of America’s Public Health System: Trends, Risks, and Recommendations, 2019
TFAH Applauds Passage of Senate Farm Bill
(Washington, D.C., June 29, 2018) – John Auerbach, president and CEO, of Trust for America’s Health (TFAH) today made the following statement regarding Senate passage of “Farm Bill” legislation (the Agriculture Improvement Act – Senate amendment to H.R. 2) to reauthorize key federal agricultural and nutrition programs.
“The Trust for America’s Health is pleased the U.S. Senate has completed work on Farm Bill legislation that will support and promote good nutrition and improved health outcomes. By rejecting the approach taken by the House, the Senate bill largely protects and strengthens the Supplemental Nutrition Assistance Program (SNAP), which serves as a critical lifeline to millions of American children and families that otherwise lack the means to access adequate nourishment and make healthy food choices.
In addition to increases in funding to the Food Insecurity Nutrition Incentive Pilot, the Senate bill includes a Harvesting Health pilot that would help to further promote linkages between health care providers and anti-hunger and nutrition improvement activities.
According to TFAH’s State of Obesity report, roughly two out of every three adults or one out of every three children is either obese or overweight. Obesity remains both a significant public health crisis and a national security issue-being overweight or obese is the leading cause of medical disqualifications for military service, with nearly one-quarter of applicants being rejected for exceeding the weight or body fat standards. Additionally, obesity translates to higher health care costs and poor quality of life.
Many efforts are underway that encourage SNAP recipients to make healthy food choices; for example, incentive programs to use SNAP benefits at farmers’ markets. Such efforts, combined with other prevention programs and policies, have been shown to be effective. We must now continue to invest in and scale such approaches to help Americans eat healthier. SNAP and other Farm Bill programs will be critical to turning the tide against this longstanding health problem.
TFAH looks forward to continuing to work with Congress through the conference process as it develops a final Farm Bill that will lead us in the right direction, towards improving the health and prosperity of all Americans.”
# # #
Trust for America’s Health is a non-profit, non-partisan organization dedicated to saving lives by protecting the health of every community and working to make disease prevention a national priority.