Pain in the Nation: The Drug, Alcohol and Suicide Crises and Need for a National Resilience Strategy
This report examines the set of epidemics the country is facing as drug overdose, alcohol-related and suicide deaths are all increasing. The report includes evidence-based programs and policies to address these triple crises.
This report is supported by grant from the Well Being Trust.
Executive Summary
The United States is facing a new set of epidemics: More than 1 million Americans have died in the past decade from drug overdoses, alcohol and suicides (2006 to 2015). In 2016, U.S. life expectancy decreased for the first time in two decades, and these three public health crises have been major contributing factors to this shift.
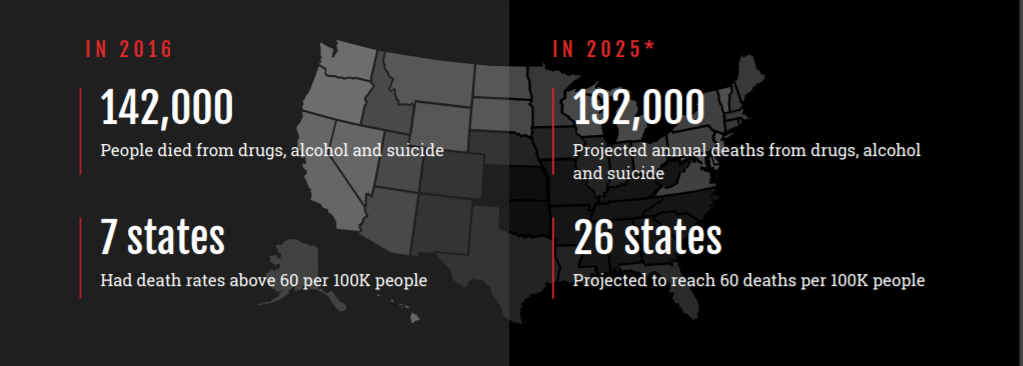
If current trends continue, drugs, alcohol and suicide could kill an estimated 1.6 million Americans between 2016 and 2025, according to a new analysis conducted by the Berkeley Research Group (BRG) for this report. That’s a 60 percent increase. Yet that estimate may be conservative, given the growth in the use of heroin, fentanyl and carfentanil. If the nation continues along recent trajectories, death rates could double to 2 million by 2025.
In 2015 alone, 127,500 Americans died from drug- or alcohol-induced causes or suicide.2 That equates to 350 deaths per day, 14 deaths per hour or one death every four minutes.
These trends are a wake-up call to a national well-being crisis. In stark terms, they are signals of serious underlying concerns facing too many Americans — about pain, despair, disconnection and lack of opportunity — and the urgent need to address them.
While these crises have received much attention, this report finds that the actions taken to date have been severely inadequate. And, if effective action is not taken, these trends could become significantly worse.
In this report, the Trust for America’s Health (TFAH) and Well Being Trust (WBT) call for development of a national strategy to improve resilience in the United States. The report examines current trends and evidence-based and expert-recommended policies, practices and programs to take a more comprehensive approach to counter these crises.
A nation in pain
For several states, the outlook posed by these threats is even more concerning:
- As of 2015, death rates from drugs, alcohol or suicide were 60 per 100,000 residents or higher in five states. New Mexico had the highest rate, 77.36 per 100,000 residents, with New Hampshire, West Virginia and Wyoming following at rates between 60 and 70 per 100,000.
- By 2025, 26 states are projected to reach death rates of 60 or more per 100,000, and two states (New Mexico and West Virginia) could reach 100 deaths per 100,000.
Recently, the opioid crisis has gained urgent national attention. Many of the strategies for addressing the opioid epidemic have focused on trying to limit the supply of prescription and illicit forms of opioids, along with measures to respond to overdoses and attempts to address major gaps in the country’s substance use disorder treatment capabilities.
However, these efforts alone will not succeed without corresponding efforts to address the broader issues that contribute to adverse well-being and underlying pain. The rise of multiple “despair deaths” and related trends show there is a more significant dynamic that must be addressed.
Many factors contribute to drug and alcohol misuse and suicide, including family and social relationships, social-emotional development, early childhood trauma and “lack of economic opportunity, poor working conditions and eroded social capital in depressed communities, accompanied by hopelessness and despair.” In addition, causation works in both directions: Substance misuse and untreated mental health issues can adversely impact health, academic and career attainment, relationships with family and friends and personal connectedness within a community.
Current and Projected Crisis Trends
Drug-related deaths
Drug-related deaths have tripled since 2000 and were responsible for more than 52,400 deaths in 2015. More than 33,000 of these deaths were from opioids, mainly prescription opioids (pain reducers), heroin and fentanyl.
- 7.7 million Americans (2.9 percent) have a drug use disorder.
- Fentanyl-related deaths increased 72.2 percent and heroin-related deaths increased 20 percent between 2014 and 2015. In 2016, data indicate that fentanyl became the leading cause of drug overdoses, at 21,000 overdose deaths, double the number in 2015.
Alcohol-induced deaths
Alcohol-induced deaths grew by 37 percent from 2000 to 2014, with 33,200 Americans dying from liver diseases, alcohol poisoning and other diseases as of 2015, a 35-year high. The rate for all alcohol-attributable deaths, including alcohol-related motor vehicle, violence and other fatalities, totals 88,000 a year.
- 15.7 million American (5.9 percent) have an alcohol use disorder.
Suicides
Suicides increased by 28 percent from 2000 to 2015, accounting for more than 44,000 deaths a year. Although suicide rates are higher among men, the highest increases have been among middle-aged women (63 percent increase) and girls ages 10 to 14 (200 percent increase).
- Alcohol use is involved in 23 percent of suicides and 40 percent of suicide attempts. Sixteen percent of suicides are from poisoning (including drug overdoses).
While overall death rates are higher among Blacks and other people of color, substance misuse and suicide are leading drivers of lowered U.S. life expectancy for the first time in decades, with an especially unprecedented increase in mortality among middle-aged Whites in the past 15 years.
- Life expectancy rates declined 20 percent among middle-class Whites with less than a college education, with deaths from drug overdoses, alcohol poisoning, liver disease and suicide all tripling among this cohort. These trends have not been seen within other racial and ethnic groups.
Mental Health and Substance Use Disorders
Mental Health and Substance Use Disorders: In 2016, 44.7 million American adults experienced a mental health issue, 20.1 million experienced a substance use disorder and 8.2 million experienced both. These numbers are likely to be underestimated due to issues of stigma.
- As many as one in five children and teens has had a serious debilitating mental disorder, with half of mental health conditions starting by age 14. More than 25 percent of teens are impacted by at least mild symptoms of depression.
- Only around one in 10 people (10.6 percent) who needed substance use treatment received the recommended treatment at a specialty facility in 2016. Four in nine adults with any mental illness received mental health services.
Chronic Pain
Chronic Pain: The National Academy of Medicine (NAM) estimates that 100 million Americans experience chronic pain. Millions more experience acute pain from injury, disease or medical procedures, while millions of others experience mental, emotional and other psychological forms of pain.
Adverse Childhood Experiences
Adverse Childhood Experiences: Across all socio-economic levels, two-thirds of Americans report having experienced an adverse childhood experience (ACE) while growing up. Nearly 40 percent experienced two or more ACEs, and 22 percent experienced three or more ACEs.
- Growing up in an environment where a family member has a mental illness or alcohol or drug use disorder can have lifelong health consequences, with the impact strongest on infants and toddlers.
- Children whose parents misuse alcohol and other drugs are three times more likely to be abused and more than four times more likely to be neglected than children from non-substance-misusing families. This in turn increases the risk that they will develop anxiety disorders and severe personality disorders and misuse alcohol and drugs themselves.
- Parents who misuse alcohol or other drugs are more likely to have multiple sources of stress, including low socio-economic status, lack of social support and resources, financial or emotional distress and mental health problems such as depression, or to have experienced abuse when they were growing up.
Consequences of Persistent and Prolonged Stress
Consequences of Persistent and Prolonged Stress: One in five babies and toddlers (around 23 percent) lives below the poverty line, and 45 percent are in low-income families.38 Children who grow up in poverty are more likely to remain poor as adults, attain lower levels of education and employment and have worse mental and physical health.
Maltreatment of Children
Maltreatment of Children: More than 680,000 children experience severe forms of maltreatment annually (79 percent from neglect and 18 percent from physical abuse); one-third of these are children under age 4. Around 400,000 are in out-of-home foster care at any time. Of these children, more than 60 percent of infants and 40 percent of older children are from families with active alcohol or drug misuse.
A National Resilience Strategy
The United States has long struggled to identify effective approaches for promoting positive mental and behavioral health and managing all forms of pain. The rise of “despair deaths” is directly related to pervasive issues with how we view and manage mental health, pain and despair. As this report shows, without better strategies that focus on building resilience by preventing problems and providing effective support, services and treatment, these trends will only get worse.
We need a comprehensive National Resilience Strategy that focuses on prevention, early identification of issues and effective treatment. Such a strategy should prioritize investing in prevention, promoting healthy communities and raising a mentally and physically healthier generation of kids. Focusing on preventing problems and providing support can help Americans thrive, with proven results for improving mental and physical health and school and career achievement. These types of approaches also provide a sound financial investment, with many prevention programs yielding positive returns on investments ranging from $3.80 to $34 for every dollar invested.

This report offers a critical look at both past and projected impacts and outcomes of opioid and alcohol misuse, including overdoses and death by suicides. It presents a scan of the evidence and a summary of the fragmented and often inadequate constellation of existing national policies and programs to address these pressing issues.
One thing is clear: There is an immediate need to develop an actionable national response to alcohol and drug misuses and death by suicide.
Not only are these urgent health crises across this country, they are indicators of the need to go deeper and to look at underlying causes and opportunities to create an integrated approach to well-being for all people, and especially for those who are at a high risk for experiencing these challenges. The findings of this report serve as a call to action from leaders across all sectors and regions/states to come together to develop a thoughtful and inclusive framework for systemic change that measurably improves outcomes tied to well-being and health.
There must be a paradigm shift in the response to these challenges, with top priorities that include:
Improving Pain Management and Treatment.
The opioid epidemic demonstrates the need to improve how the country views and manages pain. There is both a cultural need to better understand pain and its impacts and a need within the healthcare system to develop and support different pain treatment approaches and to provide ongoing training for responsible prescription opioid prescribing practices. People need physical, emotional and mental healing.
Specific Actions to Stem the Opioid Crisis.
A full-scale approach must include promoting responsible opioid prescribing practices (such as provider education and best practices for prescription drug monitoring programs); public education about misuse and safe disposal of unused drugs; “hotspot” intervention strategies; anti-trafficking to stop the flow of heroin, fentanyl and other illicit drugs; and expanding the use and availability of rescue drugs, sterile syringes and diversion programs.
Specific Actions to Reduce the Alcohol Crisis.
Evidence-based approaches to reduce excessive drinking include increasing alcohol prices, limiting hours and density of alcohol sales and enforcing underage drinking laws, such as by holding sellers and hosts liable for serving minors.
Specific Actions to Reduce the Suicide Crisis.
Support suicide prevention plans in states, schools and health systems, including crisis intervention services; training teachers, employers, community leaders, faith-leaders and others to identify and support those at-risk; and anti-bullying and social-emotional learning and supports in schools.
Focusing on the Impact on Children and the Need for a Multi-Generational Approach to Resilience.
The opioid crisis demonstrates the intergenerational impacts of behavioral health issues and the urgent need to address these effects on children. Solutions must focus on providing support not only for the person with a substance use disorder but also for the children, parents and families who are affected. The epidemic is creating a new, compounded and complicated generation of ACEs, which have long-term effects on children’s lives. Tweens and teens are coming of age with new and different substance misuse risks for prescription opioids, heroin and heroin mixed with other drugs. Family and community influences also increase the risk for a child’s future misuse of alcohol and for both suicidal thoughts and suicide. Systems and supports must be aligned to support family needs, from providing support for prevention and treatment to programs that teach in-home parenting skills and strategies that strengthen and keep families together when possible.
Putting Prevention First.
A multi-generational system must include a coordinated, effective system for supporting children and families. Experts have identified a broad range of effective policies and programs that reduce substance misuse, suicide and promote resilience by reducing risk factors and supporting positive protective factors (such as stable, secure families, homes and communities). These programs, however, are often ad hoc and are not provided at scale or coordinated to achieve maximum results for families.
New models and infrastructure are needed that support better alignment, integration and case management of services and supports for families across healthcare, behavioral health services and other social services. There also needs to be support for community-based efforts that address the opioid, alcohol and suicide crises and improve well-being. It will be critical to address these issues in ways that effectively use the expertise and resources of local institutions and businesses and bring together community leaders to support improved social connectedness and economic opportunity.
Focus on Early Childhood.
Investing in early childhood policies and programs will have the biggest impact for reducing risks and supporting a lifetime of better well-being. Key factors include: nurturing, stable caretakers and relationships; good nutrition and physical activity; positivelearning experiences; a safe home, neighborhood and environment; and high-quality, preventive healthcare. Early intervention to prevent issues can help avoid a “cascade of risk,” including the multi-generational impact of adverse experiences.52 Improved systems are needed to coordinate the services and supports available to children and families at risk, helping to identify problems early and ensure families receive necessary care. Some impactful early childhood programs include: high-quality home visiting programs, evidence-based parent education and support, high-quality child care and early education and services that support the transition from early childhood programs to elementary school. It is also important to provide support for families to improve their stability and resilience, including financial, food, housing and transportation assistance and quality healthcare.
Reboot School-Community Efforts to Support Tweens and Teens.
There is significant evidence on the effectiveness of approaches for improving well-being during the tween and teen years, when many young people face significant transitions, including changes in schools and relationships, and when mental health concerns become evident and risks for substance misuse may emerge. Yet many effective programs have never been widely implemented. A real commitment must be made to supporting evidence-based prevention efforts among school-aged children and youth, moving past years of ineffective or non-existent school-based efforts. Some key strategies include: school-community connected efforts; social-emotional learning and life and coping skills; positive and inclusive school environments; anti-bullying efforts; training for educators and other “gatekeepers” to help identify when youth are at-risk; increasing the number of school counselors, mental health personnel and health services; and screening, early intervention and connection to appropriate services as needed.
Increasing Access to Expert Advice and Support: Establishing Expert Networks.
Communities struggling with opioid and related epidemics must be able to access experts to better inform their decisions about the most effective, evidence-based and promising strategies available to them. They should also be able to receive technical assistance and evaluation supports to ensure that their efforts are well-implemented and achieve results. Currently, federal agencies and philanthropies offer some resources. However, most states and communities do not have this type of access to expert assistance and support. Creating state-level support and advisory centers would ensure that communities can tap into assistance from leading academic and government experts and focus more effectively on improving well-being and health. Successful models for developing this type of network include Communities That Care and EPIS Center.
Achieving Parity and Integration: Improving and Expanding Behavioral Health Services and Aligning with Healthcare to Support the “Whole Health” of Individuals and Families.
Over the past two decades, federal and state policies shifted to recognize the need to provide mental health and substance use disorder treatment (often combined to be referred to as behavioral health) on parity with the level of treatment for physical health problems. The persistence of legacy systems, views and approaches, however, makes achieving parity and integration a challenge. Mental health and substance use disorders traditionally have been treated through separate systems. A concerted effort is needed to expand availability of and access to behavioral health services and coverage, reform payment models and improve service delivery systems and workforce models, including those integrated with or connected to primary healthcare. It is particularly important to develop for systems for improving care delivery and quality in communities, both rural and urban, where options for behavioral healthcare are limited or non-existent. Expanding the availability and quality of services also means supporting new models for delivery, such as telehealth and other innovative practices, and increasing workforce development initiatives and greater use of community health workers and peer-counselor/support models where appropriate.
Early Identification of Issues and Connection to Supports and Services.
Supporting “whole health” requires supporting systems that identify problems early and connect people to the services they need. This includes improved case management and connection to social service supports that can have a significant impact on health. Several effective tools identify children and families at risk, as well as tweens, teens, youth and adults at risk for substance misuse, mental health concerns and suicide. Models like Accountable Health Communities and Nurse Family Partnerships help support systems for identification, referral, connection to care and follow-up.
Conclusion
The United States is in a crisis of pain, despair and disconnection. If current trends continue, drugs, alcohol and suicide will kill up to an estimated 1.6 million Americans between 2016 and 2025.
Strong, concerted and immediate action is needed to counter rising opioid, alcohol and suicide death rates and address the underlying pain, prolonged stress, hopelessness, financial insecurity and other factors contributing to these trends.

This report urges leaders across all sectors, regions and states to come together to develop a National Resilience Strategy, a thoughtful and inclusive framework for systemic change that measurably improves outcomes tied to well-being and health for all people, and especially those at high risk. Such a strategy should prioritize investing in prevention and early identification of problems, promoting healthy communities and raising a mentally and physically healthier generation of kids. Focusing on preventing problems and providing support can help Americans thrive, with proven results for improving mental and physical health and school and career achievement.
To assist in this effort, a broad range of evidence-based and promising policies and programs are available to tackle the rising tide of drug, alcohol and suicide deaths. These include ways to focus on preventing problems in the first place as well as modernizing and expanding the behavioral health system to focus more broadly on “whole health,” to treat and manage pain more effectively and to build resilience across generations.



