Public health agencies can play vital role in supporting caregivers
(Washington, DC – September 30, 2025) – As the percentage of older adults continues to grow in the United States, so do the number of people providing informal caregiving to them. A new policy brief highlighting the role of caregivers, published by Trust for America’s Health (TFAH) today, finds that many people who provide unpaid, informal caregiving are experiencing increasing levels of economic, emotional, and physical hardships as a result. The brief highlights the many roles that public health agencies can play in supporting caregivers and that more federal and state interventions are needed to support this growing segment of the population.
The brief, Public Health’s Roles in Supporting Informal and Family Caregivers, reports that 41.8 million people served as a caregiver to an adult over the age of 50 in 2020, an increase of over 7 million people who provided unpaid care to a family member or friend in 2015.
“The prevalence of caregiving in the U.S. has grown exponentially more complex,” said Megan Wolfe, senior policy development manager at TFAH who leads its Age-Friendly Public Health Systems initiative. “As more jurisdictions work to be age-friendly communities, having a nuanced understanding of the role and challenges facing caregivers will allow public health organizations to work with community partners to advocate for and provide the support caregivers need.”
The caregiving population is a diverse one, with about 40 percent of caregivers being individuals of color (17 percent Hispanic or Latino, 14 percent non-Hispanic Black, 5 percent Asian American and Pacific Islander, and 3 percent some other race/ethnicity, including those who identified as multiracial), according to the brief.
Women that serve as caregivers and caregivers of color face greater financial stress and physical demands that can impact their health, including experiencing depressive symptoms and feeling ignored or difficulty navigating healthcare systems.
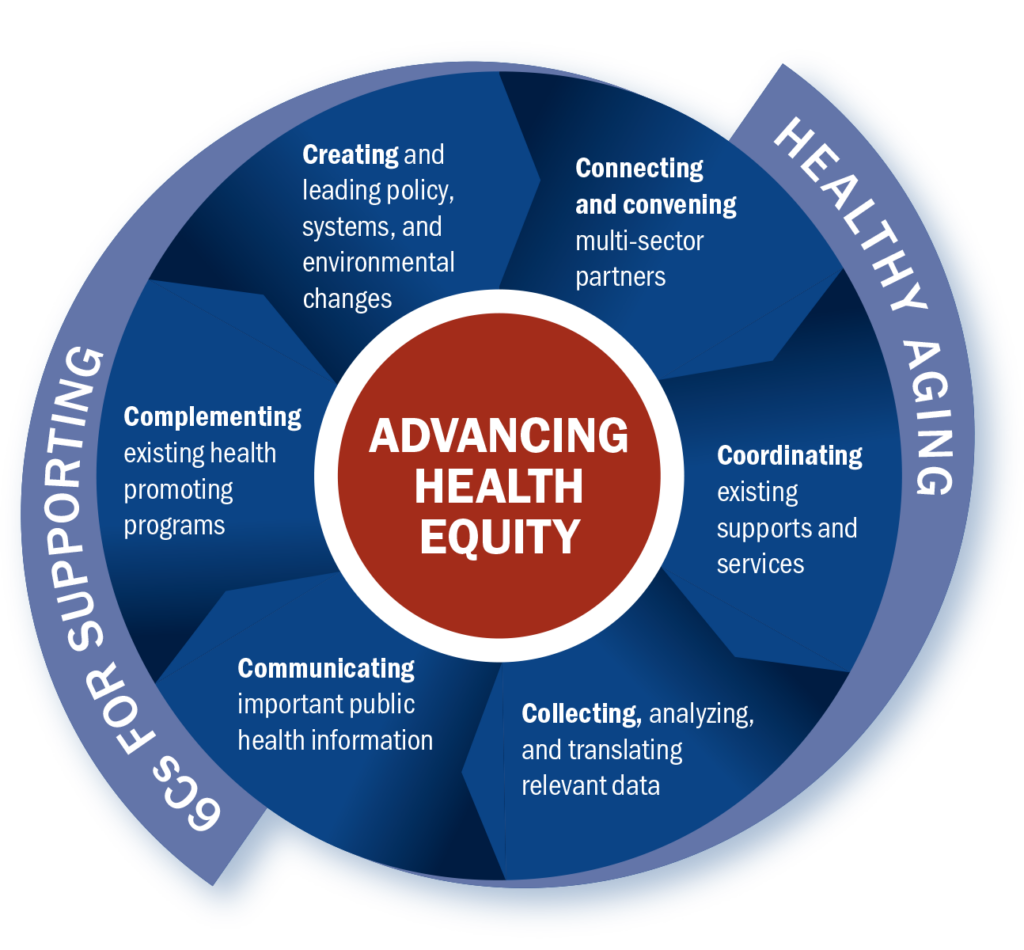
TFAH’s Age-Friendly Public Health Systems (AFPHS) provides guidance for public health practitioners on the policy and systems changes that are needed to advance healthy aging and build supportive communities. This includes programs and activities that support caregivers, including better availability and easier navigation of caregivers’ supports.
The brief provides recommendations for the roles of public health that are aligned with the AFPHS Framework, including:
- Advocate for changes to the workplace to create supports for caregivers including leave policies and employment protections.
- Help create cross sector initiatives that support older adult and caregiver needs.
- Work with the healthcare sector to ensure that healthcare providers understand and can refer caregivers to non-clinical support resources in their communities.
- Collect data on the experience of caregivers and help communities design programs that meet their needs.
- Model the use of culturally appropriate communication strategies that recognize the diversity of the caregiving population.
- Create programs that provide caregivers with the tools they need to care for themselves and their care recipients.
TFAH’s Age-Friendly Public Health Systems initiative is made possible with generous support from The John A. Hartford Foundation.
To learn more about the Age-Friendly Public Health Systems initiative, visit Age-Friendly Public Health Systems – Trust for America’s Health (afphs.org)
# # #
Trust for America’s Health is a nonprofit, nonpartisan public health policy, research, and advocacy organization that promotes optimal health for every person and community and works to make the prevention of illness and injury a national priority.
The John A. Hartford Foundation, based in New York City, is a private, nonpartisan, national philanthropy dedicated to improving the care of older adults. The leader in the field of aging and health, the Foundation has three areas of emphasis: creating age-friendly health systems, supporting family caregivers and improving serious illness and end-of-life care. https://www.johnahartford.org/





 According to the latest edition of Trust for America’s Health’s
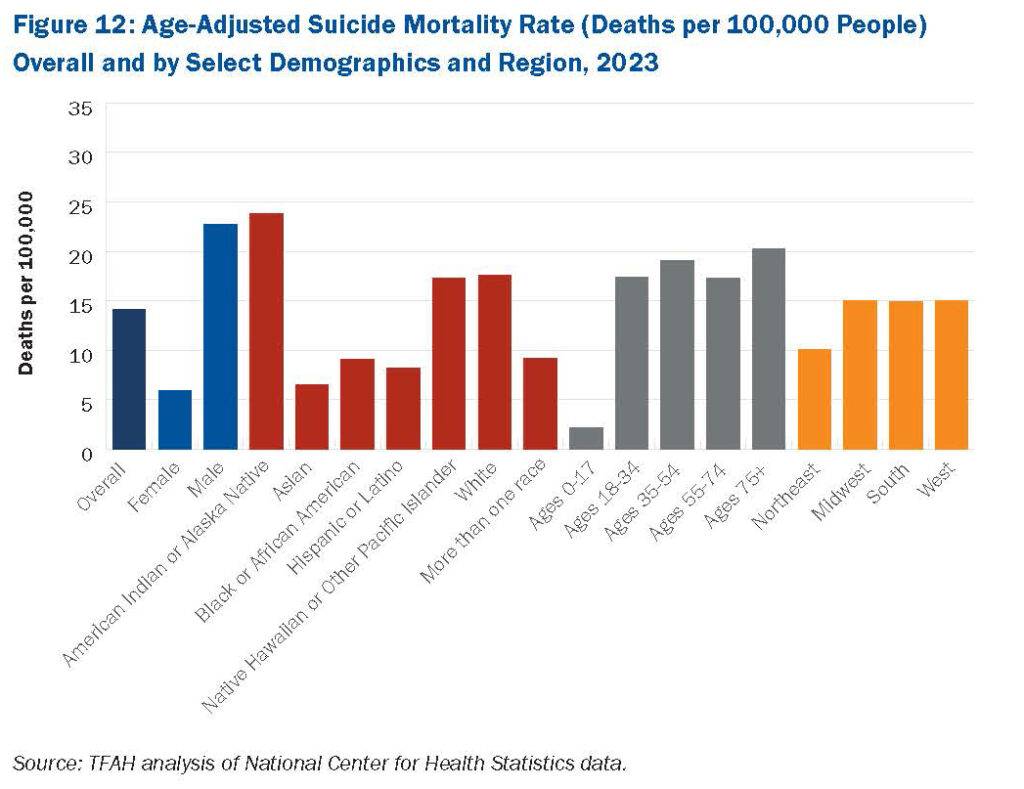
According to the latest edition of Trust for America’s Health’s  Some of the highest age-adjusted suicide rates are seen in males and adults ages 75 and older. Suicide rates in
Some of the highest age-adjusted suicide rates are seen in males and adults ages 75 and older. Suicide rates in 
 Megan: The Guide can be used by anyone who wants to build expertise in healthy aging, especially from a public health perspective. Our vision is that entire health department staffs will use it, but it’s also perfect for individuals or small teams to work through together.
Megan: The Guide can be used by anyone who wants to build expertise in healthy aging, especially from a public health perspective. Our vision is that entire health department staffs will use it, but it’s also perfect for individuals or small teams to work through together.