Datos demuestran una Primera Mejoría en Cinco Años, en la Tasa de Mortalidad Combinada por Abuso de Sustancias y Suicidio, pero las Tendencias de Varias Décadas Siguen siendo Alarmantemente Altas
(Washington, DC – 31 de julio de 2024) – Una disminución en la tasa de mortalidad inducida por alcohol llevó a una tasa combinada ligeramente más baja de todas las muertes en EE. UU. debido al alcohol, drogas y suicidio en 2022, pero la tendencia a largo plazo de tales muertes sigue siendo alarmantemente alta, según un informe publicado hoy por Trust for America’s Health (TFAH, por sus siglas en inglés).
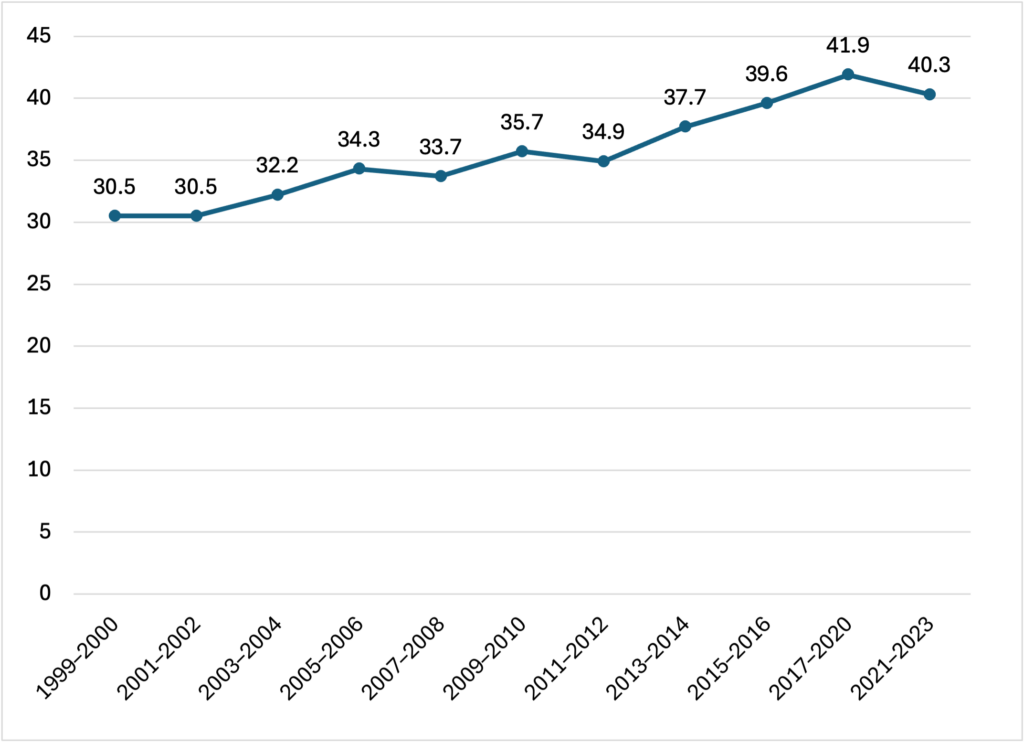
El informe Pain in the Nation 2024: La Epidemia de Muertes por Alcohol, Drogas y Suicidio, incluye datos que muestran que entre 2002 y 2022, la tasa combinada de muertes por alcohol, drogas y suicidio ha aumentado en un 142 por ciento, con 74,003 muertes registradas en 2002 a 207,827 muertes en el 2022.
En 2022, la tasa de mortalidad inducida por alcohol disminuyó en un seis por ciento registrando 13.5 muertes por cada 100,000 personas, la primera disminución en la tasa después de más de una década de aumentos, pero las tasas de muertes por sobredosis de drogas y suicidio no presentaron ningún cambio, permanecieron iguales.
Las tasas y tendencias de muertes por abuso de sustancias y suicidio varían entre grupos de población, estados y regiones del país. Las personas indígenas americanas, nativas de Alaska, las personas negras y las personas blancas tienen tasas combinadas más altas que el promedio de muertes por alcohol, drogas y suicidio, mientras que las personas asiáticas, latinas, personas multirraciales, nativas hawaianas y de otras islas del Pacífico, tienen tasas más bajas que el promedio de muertes por abuso de sustancia y suicidio.
En 2002, los estados con las tasas más altas de muertes por alcohol, drogas y suicidio eran Nuevo México con 124.3 muertes por cada 100,000 personas, Virginia Occidental con 115.7 muertes por cada 100,000 personas y Alaska registrando 104.1 muertes por cada 100,000 personas.
El Uso de Sustancias y Sobredosis de Drogas
La tasa de mortalidad por sobredosis de drogas, cifras entre todas las edades, se mantuvo en general sin cambios entre el 2021 al 2022 con 32.4 muertes por cada 100,000 personas y de 32.6 muertes por cada 100,000 respectivamente, pero a pesar de la tendencia 107,941 personas murieron en EE. UU. debido a una sobredosis de drogas en el 2022.
Según los datos recopilados por la Administración de Servicios de Salud Mental y Abuso de Sustancias de EE. UU., en el 2022, demuestra que aproximadamente 70 millones de personas en EE. UU. de 12 años o más, alrededor de una cuarta parte de la población adolescente y adulta, reportaron haber consumido una o más drogas ilegales, mientras que poco menos del 10 por ciento de las personas a partir de los 12 años en adelante en EE. UU. tenían un trastorno tras el uso de drogas.
Las tasas de sobredosis de drogas fueron más altas entre las personas indígenas americanas/nativas de Alaska con 65.2 muertes por cada 100,000 personas, los adultos de 35 a 54 años registraron 59.4 muertes por cada 100,000, las personas negras con 47.5 muertes por cada 100,000 y los hombres con 45.6 muertes por cada 100,000.
Abuso del Alcohol
El abuso de alcohol, a pesar de que hubo una disminución de muertes inducidas por alcohol en 2022, se registraron 51,191 personas que murieron por causas inducidas por alcohol durante el año en EE. UU. Las muertes inducidas por alcohol fueron más altas entre las personas indígenas americanas y nativas de Alaska, con una tasa de 78.4 muertes por cada 100,000 personas, y los adultos de 55 a 74 años con 34.9 muertes por cada 100,000 personas.
Muertes por Suicidio
En el 2022, 49,476 personas. murieron a causa de suicidio en EE. UU. La mortalidad general por suicidio se mantuvo prácticamente sin cambios entre 2021 y 2022, con 14.1 muertes por cada 100,000 personas y 14.2 muertes por cada 100,000 respectivamente.
La tasa más alta de suicidio fue entre las personas indígenas americanas/nativas de Alaska con 27.1 muertes por cada 100,000 personas, los hombres con 23 muertes por cada 100,000, los adultos mayores con 21 muertes por cada 100,000 y las personas que viven en áreas rurales con 20.5 muertes por cada 100,000. La mortalidad por suicidio entre los grupos de edad se movió en diferentes direcciones, con las muertes por suicidio entre los jóvenes con edades entre 0-17 y 18-34 ha ido disminuyendo, pero la mortalidad ha aumentado para todos los grupos de edad avanzada.
“Aunque la estabilización en la tasa combinada de muertes por alcohol, drogas y suicidio en 2022 es una buena noticia, está ensombrecida por décadas de aumento en el número de tales muertes y resalta la necesidad de continuar aplicando soluciones basadas en evidencia para salvar vidas”, dijo J. Nadine Gracia, M.D., MSCE, presidenta y CEO de Trust For America ’s Health. “Tenemos estrategias que sabemos que funcionan, incluyendo la prevención temprana y estrategias de reducción de daños, asegurando el acceso a la atención de salud mental y conductual, y creando condiciones comunitarias que apoyen a los niños y las familias y ofrezcan a las personas oportunidades de educación y empleo. Necesitamos invertir en estos programas.”
Recomendaciones del Reporte
El informe incluye ciertas recomendaciones para los funcionarios del gobierno federal, estatal y local, entre otros interesados, para que sigan ciertos pasos para abordar para abordar la crisis de abuso de sustancias y suicidio, estas recomendaciones incluyen:
Invertir en la prevención y en condiciones comunitarias que promuevan la salud, incluyendo programas para reducir aquellas experiencias adversas durante la niñez y aquellos que apoyen a las familias y ofrezcan programas de apoyo juvenil informados por el trauma y culturalmente apropiados.
Reducir el riesgo de sobredosis y el acceso a medios letales de suicidio a través de programas de reducción de daños, incluido los programas de servicios de jeringas, acceso a medicamentos para la prevención de sobredosis como la naloxona y promover el almacenamiento seguro de las armas de fuego.
Fortalecer el sistema de prevención de salud mental y abuso de sustancias mediante la construcción continua de programas de intervención en crisis, asegurando el acceso a servicios de salud mental y abuso de sustancias, aumentando la fuerza laboral de salud mental, incluyendo la diversidad, ofreciendo servicios culturales, adaptados a cada lengua.
Trust for America’s Health es una organización sin ánimo de lucro y no partidista que promueve una salud óptima para todas las personas y comunidades y hace de la prevención de enfermedades y lesiones una prioridad nacional. Trust for America’s Health (tfah.org)