The State of Obesity 2018: Better Policies for a Healthier America
Each year, the "State of Obesity: Better Policies for a Healthier America" report highlights the latest obesity trends as well as strategies, policies, programs, and practices that can reverse the epidemic. The report also details the level of commitment necessary to effectively fight obesity on a large scale and includes key recommendations for specific actions. This is the 15th annual State of Obesity report by TFAH and the Robert Wood Johnson Foundation.
Introduction

New studies documenting national obesity rates and trends from the past year reinforce what we already know: obesity rates are alarmingly high; sustained, meaningful reductions have not yet been achieved nationally, except possibly among our youngest children in low-income families; many populations continue to see steady increases in obesity; and racial, ethnic, and geographic disparities persist. Therefore, addressing the obesity epidemic remains imperative for ensuring the health of the nation.
Addressing the obesity epidemic remains imperative for ensuring the health of the nation.
According to the most recent National Health and Nutrition Examination Survey (NHANES), 18.5 percent of children and 39.6 percent of adults had obesity in 2015-2016. These are the highest rates ever documented by NHANES. There were no statistically significant changes in youth or adult rates compared with the 2013-2014 survey, but rates have increased significantly since 1999-2000, when 13.9 percent of children and 30.5 percent of adults had obesity.
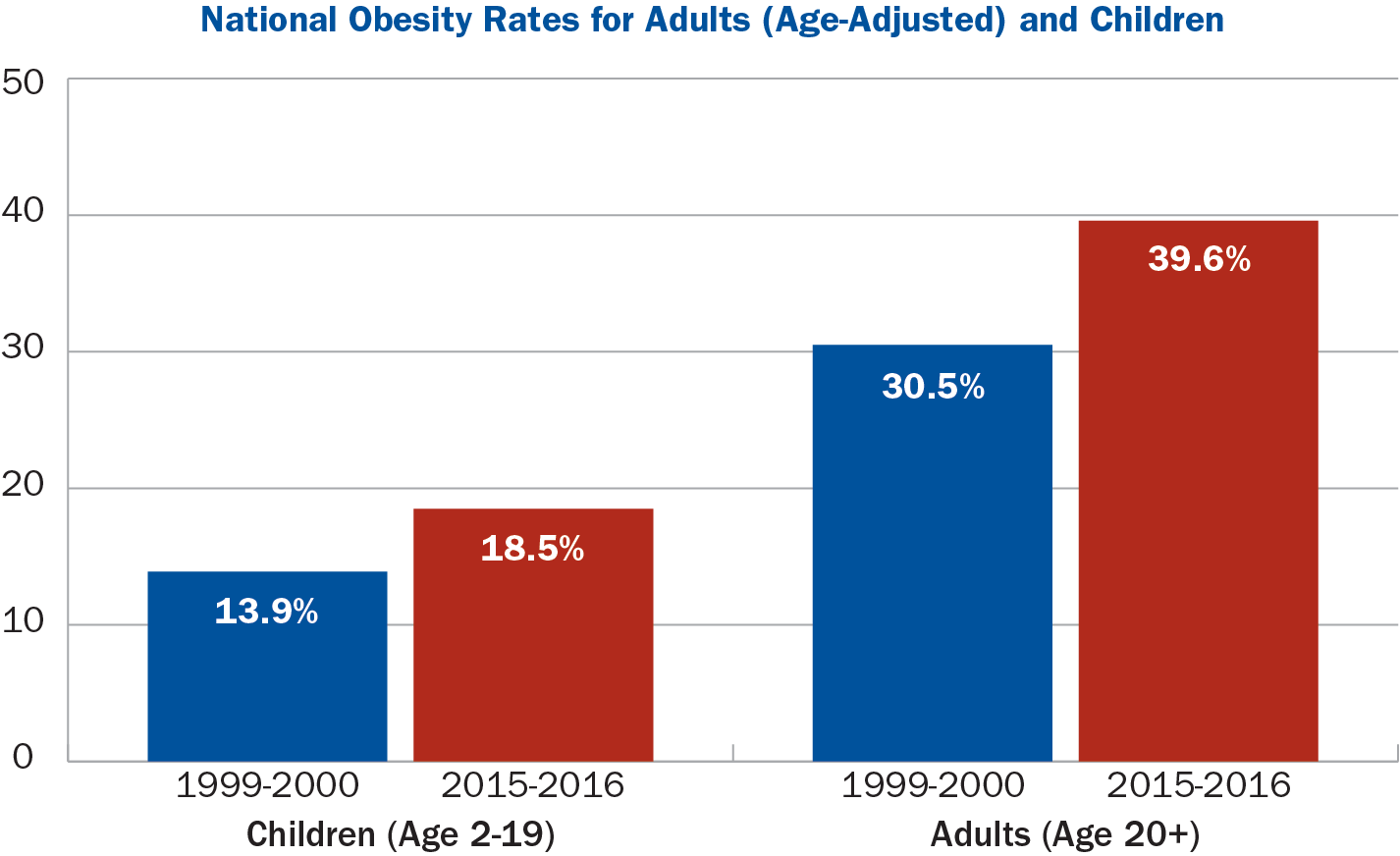 Source: NHANES
Source: NHANES
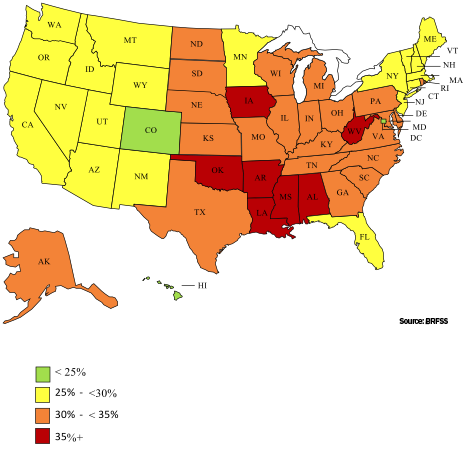
Adult Obesity Rates by State, 2017
In addition, new state level data from the CDC’s 2017 Behavioral Risk Factor Surveillance Survey (BRFSS) show that adult obesity rates rose by statistically significant amounts in six states and no states experienced a reduction in rates of obesity.
Striking disparities
The severity of racial, ethnic, and geographic disparities remains striking. Black and Latino children and adults continue to have higher obesity rates than Whites and Asians. The Youth Risk Behavior Survey, which is based on self-reported data, found that 14.8 percent of U.S. high school students had obesity in 2017. That survey also reported persistent inequities — 18.2 percent of Black and Latino high schoolers had obesity compared with 12.5 percent of their White peers. Two other studies found that adults and children who live in rural areas have higher rates of severe obesity.
While obesity rates can seem intractable, there have been some promising developments among age- and geographic-specific populations.
While obesity rates can seem intractable, there have been some promising developments among age- and geographic-specific populations. Rates of obesity and severe obesity have declined among 2- to 4-year-olds enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). From 2010 to 2014, the rate dropped from 15.9 percent to 14.5 percent nationally. The drop was geographically widespread as well: 31 states and three U.S. territories reported declines. Some communities also have documented declines in overall childhood obesity rates.
In the last year, more evidence and lessons emerged from research of policies and programs focused on addressing obesity at the individual, community, and state levels. First, the U.S. Centers for Disease Control and Prevention (CDC) shared encouraging research about a project in Texas that found an intensive, multi-sector program with a clinical focus can be successful at reducing the weight of children in low-income communities who are overweight or have obesity — but that long-term, continued support is needed, or improvement can be lost. Second, the Healthy Communities Study, which included more than 5,000 children in 1,000 communities, found that children living in localities that did more to encourage physical activity and healthy nutrition had lower body mass index and waist circumference measures. And third, a recent study found that states implementing CDC-funded nutrition and physical activity programs between 2000 and 2010 had 2.4 percent to 3.8 percent reduction in the odds of obesity among adults. Together, these studies demonstrate that states and communities that support multi-sector collaborations and innovative policy approaches over sustained periods can achieve reductions in obesity and offer models for nationwide adoption.
The Healthy Communities Study found that children living in localities that did more to encourage physical activity and healthy nutrition had lower body mass index and waist circumference measures
In addition, our analysis of new data from the 2017 Behavioral Risk Factor Surveillance System (BRFSS) shows progress on adult obesity occurring in some states. For example, adult obesity rates range from a high of 38.1 percent in West Virginia to a low of 22.6 percent in Colorado, with no state seeing improvement in its obesity rate over the past year.
Necessities for progress
Accelerating progress to address obesity will require collaboration, sufficient resources, and sustained efforts, including by federal, state, and local agencies and the private sector. For decades, experts at CDC, National Institutes of Health (NIH), U.S. Department of Agriculture (USDA), U.S. Department of Education, the Administration for Children and Families, and the Food and Drug Administration (FDA) have been researching and developing strategies to prevent and address obesity among children and adults nationwide. Over the last 15 years, policymakers took significant steps to implement new approaches through the WIC program, the Supplemental Nutrition Assistance Program, the National School Lunch and Breakfast Programs, updated menu labeling rules, and an updated Nutrition Facts label. Some of these efforts were delayed or weakened, however, preventing full implementation and thus denying researchers the ability to effectively study which efforts best help people maintain a healthy weight.
For instance, a USDA rule published in November 2017 scaled back key nutrition standards for school breakfast and lunch programs that went into effect in 2012. The question is whether schools will continue the healthy changes that they already implemented. In 23 states, 100 percent of school food agencies were compliant as of September 2016 and at least 90 percent of agencies were compliant in every state. FDA requirements for food retailers and restaurants to post calorie information on menus and elsewhere went into effect in May 2018, more than eight years after becoming law and after several unnecessary delays. Recent federal budget proposals include deep cuts to key health programs such as the CDC’s National Center for Chronic Disease Prevention and Health Promotion. This cut would eliminate dedicated funding for addressing nutrition, physical activity, and obesity.
Limiting policies and funding for obesity-prevention efforts at a moment when the enormity and intractability of this public health problem is so pressing will have adverse consequences for the country and its residents.
Limiting policies and funding for obesity-prevention efforts at a moment when the enormity and intractability of this public health problem is so pressing will have adverse consequences for the country and its residents. After all, Americans’ health is directly tied to national security and the U.S. economy.
In response to ongoing high levels of obesity, the United States must be bold enough to find and test new strategies, and resolute enough to intensify evidence-based solutions that are already making a difference. This means communities, governments, and other institutions need to work across sectors and levels to support policies, practices, and programs that work. Over time, these investments can pay off — in lives saved and in reduced healthcare costs.
Recommendations
The annual State of Obesity reports have documented how, over the past 15 years, a series of evidenced-based policies and programs have helped Americans eat healthier and provided more opportunities for physical activity in their homes, schools, and communities. These initiatives have taken root at the local, state, and federal levels, with participation from the private sector.
The impact has been substantial:
- More than 30 million children eat healthier school breakfasts, lunches, and snacks thanks to the updated nutrition standards ushered in by the Healthy, Hunger-Free Kids Act of 2010.
- Major food and beverage companies removed 6.4 trillion calories from the marketplace between 2007 and 2012.
- Thirty-three states have implemented Complete Streets policies to encourage and facilitate walking and biking.
- Thirty-five states have made Healthy Food Financing Initiative investments to increase healthy food access in underserved communities.
- In 2017, new rules strengthened school wellness policies to ensure healthier food marketing in schools, and updated nutrition standards for the more than 4 million children who participate in programs associated with the Child and Adult Care Food Program
- In 2018, menu-labeling provisions of the Affordable Care Act took effect, covering approximately 300,000 food retail establishments nationwide; FDA estimates that these rules will save approximately $8 billion in health costs over the next two decades.

But, this progress is fragile, and at risk of being halted or even reversed. This is particularly troubling because sustained, meaningful reductions in obesity have not yet been achieved nationally and racial, ethnic, and geographic disparities in obesity rates persist.
A renewed commitment to prevention policies and programs, and continued innovation at the state and local levels, is critical to reducing levels of obesity among children and adults in our country. Effective obesity prevention efforts also require substantial investment to support multi-faceted, multi-sector collaborations; merging multiple sources of public and private funding can best ensure that these efforts are sustainable as a long-term enterprise. This is particularly important for populations that have elevated obesity levels and risk factors for related illnesses.
Trust for America’s Health and the Robert Wood Johnson Foundation recommend three guiding principles regarding obesity prevention:
-
Promote policies and scale programs that take a multi-sector approach.
Multi-sector, aligned initiatives — collaborations that involve, for example, health departments, schools, transportation departments, local businesses, and other agencies — are more likely to achieve results.
-
Adopt and implement policies that help make the healthy choice the easy choice.
Federal, state, and local governments can create conditions in schools, communities, and workplaces that make healthy eating and active living accessible, affordable, and convenient.
-
Invest in programs that level the playing field for all individuals and families.
While obesity affects all populations, some have significantly higher levels than others — often due to social and economic factors largely beyond their control, such as racism, poverty, and lack of access to healthcare. Carefully designed initiatives that are informed by community input and address these challenges are critically important.
 TFAH and RWJF offer the following specific recommendations to federal policymakers, state and local policymakers, the food and restaurant sectors, and healthcare providers and systems.
TFAH and RWJF offer the following specific recommendations to federal policymakers, state and local policymakers, the food and restaurant sectors, and healthcare providers and systems.
Federal Policymakers
Congress and the Administration
- Support and expand policies and programs aimed at addressing obesity at the federal, state and community levels, including programs in CDC’s Division of Nutrition, Physical Activity and Obesity; community health programs like the Racial and Ethnic Approaches for Community Health program (REACH); and programs that focus on school health in CDC’s Division of Population Health.
- Ensure that every state public health agency receives targeted support to promote healthy eating and active living. Maintain and increase obesity-related emphasis in the Prevention and Public Health Fund and support the Healthy Food Financing Initiative in the Administration for Children and Families to ensure that underserved communities have access to grocery stores.
- Maintain and strengthen essential nutrition supports for low-income children, families, and individuals through programs like the Supplemental Nutrition Assistance Program (SNAP) and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). And, expand programs and pilots to make healthy foods more available and affordable for more families.
U.S. Department of Agriculture
- Maintain nutrition standards for school meals that were in effect prior to USDA’s interim final rule from November 2017, as well as current nutrition standards for school snacks.
- Continue to implement the Community Eligibility Provision that allows schools in high-poverty areas to serve free meals to all students, regardless of family income.
- Support and implement local school wellness policy rules, including the provision that all foods and beverage advertisements on school campuses meet Smart Snacks nutrition guidelines.
- Expand and evaluate pilots and programs aimed at increasing consumption of fruits, vegetables, and other healthy foods under SNAP and other nutrition programs.
- Continue to ensure that WIC provides mothers, infants, and young children with access to affordable, healthy food, and breastfeeding support.
U.S. Department of Health and Human Services
- In partnership with the U.S. Department of Agriculture, ensure that the 2020-2025 Dietary Guidelines for Americans reflect the latest and best nutrition science and including developing recommendations for children ages 2 and under in a transparent and timely manner.
- Actively support the recommendations of Step It Up! The Surgeon General’s Call to Action to Promote Walking and Walkable Communities.
U.S. Department of Education
- Maintain the Office of Safe and Healthy Schools, as well as Title I and Title IV programs under the Every Students Succeeds Act (ESSA), through which schools can receive funding for physical education and physical activity initiatives.
- Issue regular guidance covering programs, such as early childhood programs, supported through ESSA that encourage healthy eating, opportunities for physical activity, limits on screen time, and other activities that promote health.
U.S. Food and Drug Administration
- Ensure no further delays to the implementation of the updated Nutrition Facts label, currently scheduled to begin in 2020, and encourage and provide guidance to companies that wish to utilize the updated label prior to the deadline.
- Ensure full compliance with recently implemented menu labeling rules covering chain restaurants and similar food retail establishments.
- Encourage non-chain restaurants to implement the menu labeling rules voluntarily.
State and Local Policymakers
- States should continue to meet or exceed federal nutrition standards for school meals and snacks.
- Education agencies and school districts should continue and expand flexible breakfast programs, such as second-chance breakfasts, breakfast on-the-go, and breakfasts in classrooms.
- States should ensure that all students receive at least 60 minutes of physical education or activity during each school day.
- Education agencies and school districts should continue to support local wellness plan implementation to ensure students have healthy learning environments conducive to improved school performance.
- State ESSA plans should encourage schools and partners in healthcare and public health to address childhood obesity.
- States should follow expert guidance and adopt and implement best practices for nutrition, activity and screen time requirements and regulations covering child care and day care settings, including by investment in Quality Improvement Rating Systems.
- States should support access for low-income families to targeted home visiting and community-based programs that provide families with resources and connections to parenting education, nutrition programs and other services.
- States and localities should ensure the availability of healthy food retailers in underserved communities.
- States and localities should implement evidence-based nutrition standards for foods and beverages offered in government food service and vending machines.
- States and localities should ensure all restaurant meals marketed to children meet nutrition standards, and remove sugary drinks from all restaurant children’s meals.
- States should support efforts to make Safe Routes to School programs universally available and secure state-level appropriations or Transportation Alternatives Program allocations for infrastructure and other projects.
- At the state and local level, require that all road construction and reconstruction projects adopt a Complete Streets approach, ensuring that transportation plans are safe and convenient for all users.
- States should incentivize employers and businesses to expand effective employee wellness programs to promote healthy eating and physical activity.
- States should encourage innovation by implementing and testing pilot policies that show promise.
- States should refrain from adopting preemption policies that limit the ability of local communities to improve the health of their residents.
Food and Restaurant Sectors
- Food and beverage companies should follow the American Heart Association’s guidance concerning children’s intake of added sugars as they develop, reformulate, and market foods and beverages intended for children, and adopt the updated Nutrition Facts label on all products as quickly as possible.
- Food and beverage companies should eliminate children’s exposure to advertising and marketing of unhealthy products.
- Restaurants should remove sugary drinks from all children’s meals, and ensure the meals they market to children meet minimum nutrition standards.
- Restaurants should incorporate more fruits and vegetables into menus and make healthy beverages and sides the default option.
- Non-chain restaurants should voluntarily abide by the FDA’s new menu labeling rules.

Healthcare System and Providers
- Hospitals should no longer sell or serve sugary drinks on their campuses; they should also improve the nutritional quality of meals and promote breastfeeding.
- Nonprofit hospitals should prioritize childhood obesity prevention programs as they work to meet their community benefit requirements.
- All public and private health plans should cover the full range of obesity-prevention, treatment, and management services, including nutritional counseling, medications, and behavioral health consultation.
- Medicare should encourage eligible beneficiaries to enroll in obesity counseling as a covered benefit, and evaluate its use and effectiveness. Health plans, medical schools, continuing medical education, and public health departments should raise awareness about the need and availability of these services.
- The healthcare system should extend programs that are effective in terms of cost and performance, such as the Diabetes Prevention Program (DPP) and the community health worker-clinical coordination models. Providers and payers should allocate resources to educating and referring patients to DPP and other covered benefits as appropriate.
- Public and private payers should cover value-based purchasing models that incorporate health outcome measures that incentivize clinicians to prioritize healthy weight.